Introduction:
Table of Contents
Anemia is a medical condition in which the red blood cell count or hemoglobin (Hb) is less than normal. The oxygen-carrying capacity of the blood is, therefore, decreased. Red blood cells carry hemoglobin, an iron-rich protein that attaches to oxygen in the lungs and carries it to tissues throughout the body. It is a sign, not a diagnosis. There are many kinds of anemia, each with its cause. It is characterized by insufficient erythrocytes or hemoglobin. Loss of blood is the most common cause of anemia. It can be temporary or long-term, and it can range from mild to severe. This condition leads to fatigue and intolerance to cold, which is related to lack of oxygen needed for energy and heat production, and paleness which is due to low hemoglobin content.

Types of Anemia:
- Iron deficiency anemia
- Pernicious anemia
- Sickle cell anemia
- Megaloblastic anemia
- Anemia of chronic disease
- Hemolytic anemia
- Idiopathic aplastic anemia
- Thalassemia
Epidemiology:
A moderate degree of iron deficiency anemia affected approximately 610 million people worldwide or 8.8% of the population. It is slightly more common in females (9.9%) than males (7.8%). Mild iron deficiency anemia affects another 375 million.
The prevalence of anemia among non-pregnant women in India is higher than that in other South Asian countries, a recent study published in the reputed medical journal ‘The Lancet’ has revealed. According to ‘The Lancet’, anemia affects a quarter of the global population, including 293 million (47%) children younger than 5 and 468 million (30%) non-pregnant women.
Sickle cell disease is common in regions of Africa, India, Saudi Arabia, and the Mediterranean basin. Thalassemias are the most common genetic blood diseases and are found in Southeast Asia and in areas where sickle cell disease is common.
Causes of Anemia:
Anemia, like a fever, is a symptom that requires investigation to determine the underlying etiology. Anemia occurs when blood does not have enough red blood cells. This can happen if:
- The body does not make enough red blood cells.
- Bleeding causes to loss of red blood cells more quickly than they can be replaced.
- Inherited blood disorder that results in excessive destruction of red blood cells.
Causes of Common Types of Anemia:
Common types of anemia and their causes include:
Iron deficiency:
Iron deficiency anemia is caused by a shortage of the element iron in the body. Bone marrow needs iron to make hemoglobin. Without adequate iron, the body cannot produce enough hemoglobin for red blood cells.
Hemorrhagic:
Hemorrhagic anemia is a specific type of anemia that causes because sufficient decrease in red blood cells due to hemorrhage (bleeding). Common causes are large wounds, stomach ulcers, and heavy menstrual bleeding.
Megaloblastic:
In addition to iron, the body needs folate and vitamin B12 to produce a sufficient number of healthy red blood cells. A diet lacking in these and other key nutrients can cause decreased red blood cell production. Megaloblastic anemia is marked by the appearance of very large red blood cells. This disorder is caused by incomplete formation of the red blood cell resulting in large numbers of immature and incompletely developed cells.
Pernicious:
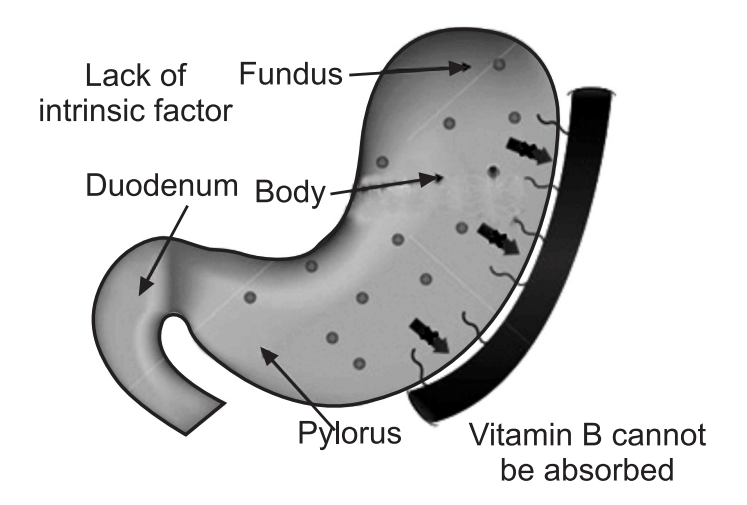
In this condition, insufficient production of RBCs results from the inability of the body to produce intrinsic factors. As a result, a person cannot absorb vitamin B12.
Pernicious anemia is a deficiency of vitamin B12 due to autoimmune attacks on the cell of the stomach and antibodies against intrinsic factors presented with megaloblastic anemia.
Chronic disease:
Certain chronic diseases such as cancer, HIV/AIDS, rheumatoid arthritis, Crohn’s disease, and other chronic inflammatory diseases can interfere with the production of red blood cells, resulting in chronic anemia. Kidney failure also can cause anemia.
Aplastic:
This is a very rare life-threatening anemia caused by a decrease in the bone marrow’s ability to produce red blood cells. Destruction or inhibition of red bone marrow results in aplastic anemia. Typically, the marrow is replaced by fatty tissues or tumor cells. Toxins, γ-radiations, certain medications, and autoimmune diseases are causes of aplastic anemia.
Associated with bone marrow disease:
A variety of diseases, such as leukemia, myelodysplasia, or myelofibrosis, can cause anemia by affecting blood production in the bone marrow. The effects of these types of cancer and cancer-like disorders vary from a mild alteration in blood production to a complete life-threatening shutdown of the blood-making process. Other cancers of the blood or bone marrow, such as multiple myeloma, myeloproliferative disorders, and lymphoma also can cause anemia.
Hemolytic:
This group of anemias develops when red blood cells are destroyed faster than bone marrow can replace them. Certain blood diseases can cause increased red blood cell destruction. If the erythrocyte cell membrane ruptures prematurely, their Hb pours out into plasma (hemolysis). The premature destruction of RBCs may result from inherent defects such as Hb defects, abnormal RBC enzymes, or defects of the RBC cell membrane. Agents that may cause hemolytic anemia are parasites, toxins, and antibodies from incompatible blood. A person can inherit a hemolytic anemia, or can develop it later in life.
Sickle cell:
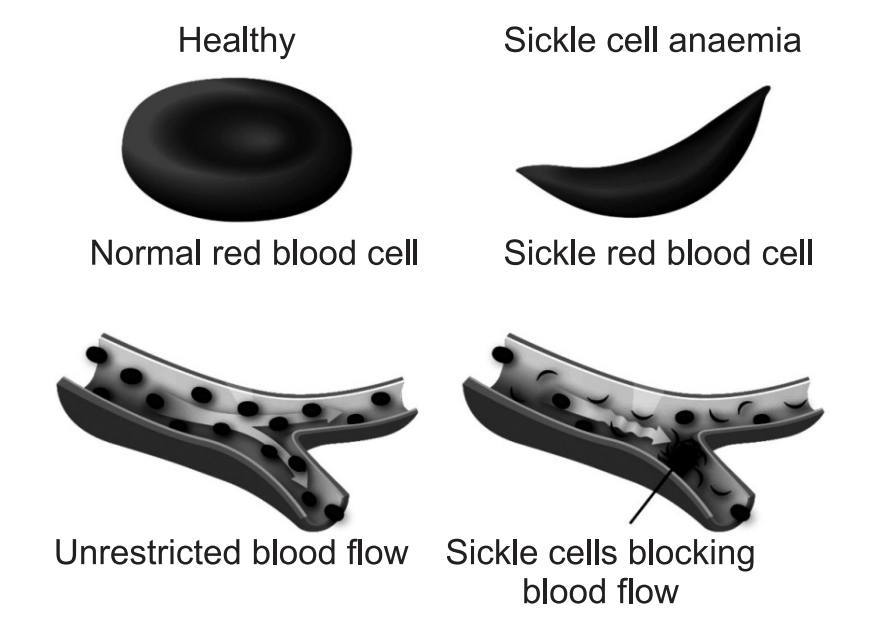
The erythrocyte of a person with Sickle Cell Anemia (SCA) manufactures an abnormal kind of hemoglobin. When such RBC gives up its oxygen to interstitial fluid, the abnormal hemoglobin tends to lose its integrity in place of low oxygen tension and forms a long stiff, rod-like structure that binds erythrocyte into a sickle shape. The sickle cell ruptures easily. Prolonged oxygen reduction may eventually cause extensive tissue damage. Furthermore, because of the shape of sickle cells, they tend to get stuck in blood vessels and can cut off blood supply to an organ altogether. SCA is characterized by several symptoms.
In young children, the hand-feet syndrome is present, in which there is swelling and pain in the wrist and feet. Older patients experience pain in the back and extremities without swelling and abdominal pain.
Other complications include neurological disorders (meningitis, seizure, stroke), impaired pulmonary functions, orthopedic abnormalities, genitourinary tract disorders (involuntary urination, blood in urine, kidney failure) ocular disturbance (hemorrhage, detached retina, blindness) convulsions, coma, and infections.
Table: Etiology and clinical features of anemias
| Anemia | Etiology | RBC Characteristics |
| Hemorrhagic | Acute blood loss. | Normocytic, normochromic, reticulocytosis. |
| Iron-deficiency. | Chronic, slow blood loss; insufficient intake relative to demands. | Microcytic, hypochromic. |
| Hemolytic Sickle cell disease Hereditary spherocytosis Autoimmune Transfusion mismatch Hemoglobinopathies Glucose-6-phosphate dehydrogenase deficiency. | Hereditary defect of RBCs; immune, infectious, mechanical, or traumatic injury of RBCs; hypersplenism. | Variable morphology in hereditary forms (e.g., sickle or spherical shape); normocytic, normochromic in other etiologies. |
| Aplastic or hypoplastic Drug-induced Radiation-induced Anemia of chronic disease Alcoholism Pernicious anemia Folate deficiency. | Hereditary or nutritional deficiency of substrate for erythropoiesis; bone marrow depression; chronic disease. | Macrocytic (megaloblastic) in substrate deficiency; normocytic, normochromic in bone marrow depression; microcytic, hypochromic in chronic disease. |
Thalassemia:
Thalassemia is a form of inherited autosomal recessive blood disorders, in which the body makes an abnormal form of hemoglobin.
Risk Factors:
Following factors lead to increased risk of anemia:
Intestinal disorders:
Having an intestinal disorder that affects the absorption of nutrients in small intestines such as Crohn’s disease and celiac disease. Surgical removal or surgery to the parts of the small intestine where nutrients are absorbed can lead to nutrient deficiencies and anemia.
Menstruation:
In general, women who have not experienced menopause have a greater risk of iron deficiency anemia than do men and postmenopausal women. That is because menstruation causes the loss of red blood cells.
Pregnancy:
In pregnancy, there is an increased risk of iron deficiency anemia because iron stores have to serve increased blood volume as well as be a source of hemoglobin for the growing baby.
Family history:
If a family has a history of inherited anemia, such as sickle cell anemia, the person may be at increased risk of the condition.
Other factors:
A history of certain infections, blood diseases and autoimmune disorders, alcoholism, exposure to toxic chemicals, and the use of some medications can affect red blood cell production and lead to anemia.
Pathophysiology of Different Types of Anemia:
[1] Pathophysiology of Iron Deficiency Anemia:
Iron is distributed to inactive metabolic and storage pools. Total body iron is about 3.5 g in healthy men and 2.5 g in women; the difference relates to women’s smaller body size, lower androgen levels, and lack of stored iron because of iron loss due to menses and pregnancy.
Iron deficiency anemia is the most common form of anemia and it develops over time if the body does not have enough iron to manufacture RBCs. Without enough iron, the body uses up all the iron it has stored in the liver, bone marrow, and other organs. Once the stored iron is depleted, the body can make very few RBCs. If erythropoietin is present without sufficient iron, there is insufficient fuel for RBC production. The red blood cells that the body can make are abnormal and do not have normal hemoglobin carrying capacity, as do normal red blood cells.
Table: Dietary sources of iron
| Dietary sources of iron |
| Heme and Non-heme iron |
| Liver |
| Meats |
| Fish |
| Poultry |
| Non-heme Iron |
| Iron-fortified infant formulas legumes |
| Eggs |
| Dairy foods |
| Wheat |
| Blackstrap molasses |
| Dried apricots |
| Raisins |
| Mustard greens |
| Strawberries |
| Tomatoes |
| Brussel sprouts |
| Broccoli |
Iron deficiency-consequences:
- Impaired physical growth,
- Compromised cognitive development,
- Impaired learning capacity,
- Reduced muscle function,
- Decreased physical activity and lower work productivity,
- Lowered immunity,
- Increased risk of infectious disease.
[2] Pathophysiology of Pernicious Anemia:
In pernicious anemia, vitamin B12 is unavailable due to a lack of intrinsic factors, a substance responsible for intestinal absorption of the vitamin B12. In a healthy person, intrinsic factor is produced by the parietal cells of the stomach. Intrinsic factor forms a complex with dietary vitamin B12 in the stomach. This complex remains intact, preventing degradation of the vitamin by intestinal juices until it reaches the ileum of the small intestine, where the vitamin is released and absorbed into the body. When an intrinsic factor is prevented from binding with vitamin B12 or when the parietal cells are unable to produce intrinsic factor, the vitamin is not absorbed, and pernicious anemia results. This is believed to stem from an autoimmune reaction in which the malfunctioning immune system produces antibodies against intrinsic factors and the parietal cells.
Without an adequate amount of vitamin B12, the body is unable to synthesize DNA properly. This in turn affects red blood cell production: the cells divide, but their nuclei remain immature, these cells are called megaloblasts. Some megaloblasts mature to become large red blood cells are called macrocytes; they reach the circulation but function abnormally. A deficiency of white blood cells (leukopenia) and platelets (thrombocytopenia) is also seen in the blood.
Pernicious anemia occurs most often in persons older than 30 years of age, although a juvenile form of the disease does occur, usually in children younger than 3 years of age.
[3] Pathophysiology of Sickle Cell Anemia:
The loss of red blood cell elasticity is central to the pathophysiology of sickle cell anemia. Normal red blood cells are quite elastic, which allows the cells to deform to pass through capillaries. In sickle cell anemia, low-oxygen tensions promote red blood cell sickling, and repeated episodes of sickling damage the cell membrane and decrease the cell’s elasticity. These cells fail to return to normal shape when normal oxygen tension is restored. As a consequence, these rigid blood cells are unable to deform as they pass through narrow capillaries, leading to vessel occlusion and ischemia.
The actual anemia of the illness is caused by hemolysis, the destruction of the red cells inside the spleen, because of their misshape. Although the bone marrow attempts to compensate by creating new red cells, it does not match the rate of destruction. Healthy red blood cells typically live for 120 days, but sickle cells only survive 10–20 days.
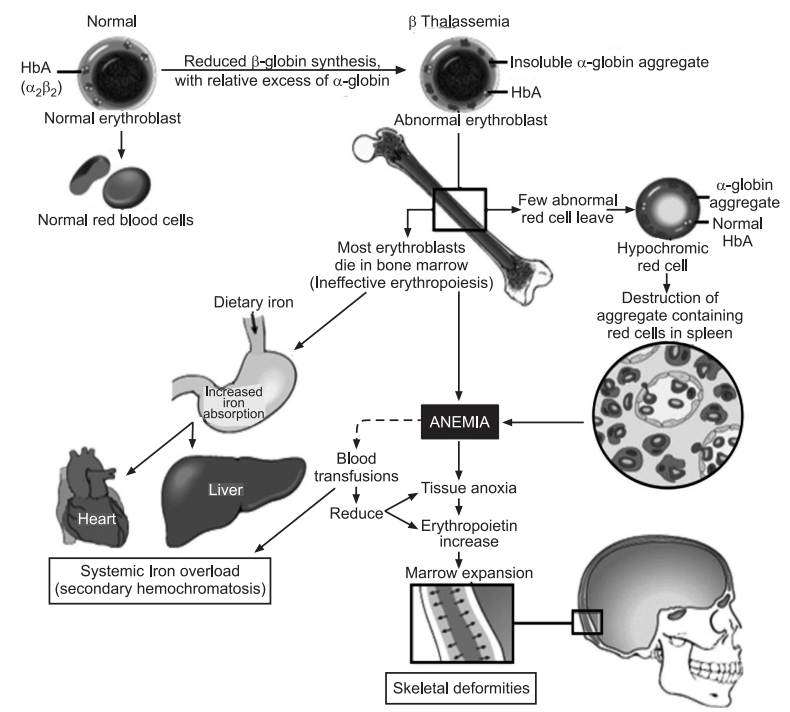
[4] Pathophysiology of Thalassemias:
Normally, the majority of adult hemoglobin (HbA) is composed of four protein chains, two α and two β globin chains arranged into a heterotetramer. In thalassemia, patients have defects in either the α or β globin chain, causing the production of abnormal red blood cells (In sickle-cell disease, the mutation is specific to β globin).
The thalassemias are classified according to which chain of the hemoglobin molecule is affected. In α-thalassemias, production of the α-globin chain is affected, while in β-thalassemia, production of the β-globin chain is affected.
Table: Features of normal and sickle RBCs
| Normal red blood cell | Sickle red blood cell |
| Structure: Smooth, flexible disk-like structure that allows it to bend and flow through the blood vessels | Structure: Sticky and stiff crescent-shaped cells causing a lack of flow through the blood vessels. |
| Function: Can flow easily through the body and carry oxygen to all the organs. | Function: Can prohibit blood flow and cause pain to the person and damage to organs. |
| Hemoglobin: Normal iron-rich protein that carries the oxygen throughout the body. | Hemoglobin: It causes the misshape and poor structure in the affected cell. |
| Recycle about every 120 days | Cells only live about 10-20 days |
The β-globin chains are encoded by a single gene on chromosome 11; α-globin chains are encoded by two closely linked genes on chromosome 16. Thus, in a normal person with two copies of each chromosome, two loci encode the β-chain, and four loci encode the α-chain. Deletion of one of the α loci has a high prevalence in people of African or Asian descent, making them more likely to develop α-thalassemia. β-Thalassemias are not only common in Africans, but also Greeks and Italians.
Symptoms of Anemia:
Anemia symptoms vary depending on the cause of anemia but may include: Fatigue, Weakness, Pale skin, a fast or irregular heartbeat, Shortness of breath, Chest pain, Dizziness, Cognitive problems, Cold hands and feet, and Headache.
Initially, anemia can be so mild it goes unnoticed. But symptoms increase as anemia worsens.
Complications:
Left untreated, anemia can cause numerous complications, such as:
Heart problems:
Anemia can lead to a rapid or irregular heartbeat (arrhythmia). The heart must pump more blood to compensate for the lack of oxygen in the blood in an anemic condition. This can even lead to congestive heart failure.
Death:
Some inherited anemias, such as sickle cell anemia, can be serious and lead to life-threatening complications. Losing a lot of blood quickly results in acute, severe anemia and can be fatal.
Tests and Diagnosis:
Physical exam:
To find out how severe anemia is and to check for possible causes includes:
- Listen to heart for a rapid or irregular heartbeat,
- Listen to lungs for rapid or uneven breathing,
- Feel abdomen to check the size of liver and spleen,
- Pelvic or rectal exam to check for common sources of blood loss.
These findings can be important clues to the underlying etiology of the disorder and provide information related to the duration of illness. The skin and mucous membranes are often bypassed, so that pallor, abnormal pigmentation, icterus, spider nevi, petechiae, purpura, angiomas, ulcerations, palmar erythema, coarseness of hair, puffiness of the face, thinning of the lateral aspects of the eyebrows, nail defects, and a usually prominent venous pattern on the abdominal wall are missed in the rush to examine the heart and the lungs.
Complete blood count (CBC):
A CBC is used to count the number of blood cells in a sample of blood. For anemia, count of the red blood cells contained in the blood (hematocrit) and the hemoglobin in the blood.
Normal adult hematocrit values vary from one to another but are generally between 40 and 52 % for men and 35 and 47 % for women. Normal adult hemoglobin values are generally 14 to 18 grams per deciliter for men and 12 to 16 grams per deciliter for women.
A test to determine the size and shape of red blood cells:
Some red blood cells may also be examined for unusual size, shape, and color. It can help to pinpoint a diagnosis.
For example, in iron deficiency anemia, red blood cells are smaller and paler in color than normal. In vitamin deficiency anemias, red blood cells are enlarged and fewer in number.
Additional tests:
Iron deficiency anemia can result from chronic bleeding of ulcers, benign polyps in the colon, colon cancer, tumors, or kidney problems.
Occasionally, it may be necessary to study a sample of bone marrow to diagnose anemia.
Treatments and Drugs of Anemia:
Anemia treatment depends on the cause.
Ferrous Sulfate Therapy:
The appropriate treatment of anemia due to blood loss is the correction of the underlying condition and oral administration of ferrous sulfate until the anemia is corrected and for several months afterward to ensure that body stores are replaced with iron. Relatively few indications exist for the use of parenteral iron therapy, and blood transfusions should be reserved for the treatment of shock or hypoxia.
Iron deficiency anemia:
This form of anemia is treated with changes in diet and iron supplements. If the underlying cause of iron deficiency is loss of blood, other than from menstruation, the source of the bleeding must be located and stopped. This may involve surgery.
Vitamin deficiency anemia:
Folic acid and vitamin C deficiency anemias are treated with dietary supplements and increasing these nutrients in the diet. If the digestive system has trouble absorbing vitamin B12 from the food the person should take vitamin B12 injections.
Anemia of chronic disease:
There is no specific treatment for this type of anemia. If symptoms become severe, a blood transfusion or injections of synthetic erythropoietin, a hormone normally produced by kidneys, may help to stimulate red blood cell production and ease fatigue.
Aplastic anemia:
Treatment for this anemia may include blood transfusions to boost levels of red blood cells. It may need a bone marrow transplant if the bone marrow is diseased and cannot make healthy blood cells.
Hemolytic anemia:
Management of hemolytic anemia includes avoiding suspect medications, treating related infections, and taking drugs that suppress the immune system, which may be attacking red blood cells.
Depending on the severity of anemia, a blood transfusion or plasmapheresis may be necessary. Plasmapheresis is a type of blood-filtering procedure. In certain cases, removal of the spleen can be helpful.
Sickle cell anemia:
Treatment for this anemia may include the administration of oxygen, pain-relieving drugs, and oral and intravenous fluids to reduce pain and prevent complications. It may also recommend blood transfusions, folic acid supplements, and antibiotics.
A bone marrow transplant may be an effective treatment in some circumstances. A cancer drug called hydroxyurea is also used to treat sickle cell anemia.
In anemias of chronic disease, associated with chemotherapy, or associated with renal disease, may require recombinant erythropoietin or epoetin alfa, to stimulate RBC production, since there is also concurrent iron deficiency and inflammation present, parenteral iron is advised to be taken concurrently.
Thalassemia:
This anemia may be treated with blood transfusions, folic acid supplements, removal of the spleen (splenectomy), and a bone marrow transplant.
Anemia associated with bone marrow disease:
Treatment of these diseases can include simple medication, chemotherapy, or bone marrow transplantation.
Prevention:
Vitamin-rich diet:
Many types of anemia cannot be prevented. However, iron deficiency anemia and vitamin deficiency anemia can be avoided by choosing a diet that includes a variety of vitamins and nutrients, including:
Iron:
Iron-rich foods include beef and other meats, beans, lentils, iron-fortified cereals, dark green leafy vegetables, and dried fruit.
Folate:
This nutrient and its synthetic form folic acid can be found in citrus fruits and juices, bananas, dark green leafy vegetables, legumes, and fortified bread, cereals, and pasta.
Vitamin B12:
This vitamin is found naturally in meat and dairy products. It is also added to some cereals and soy products, such as soya milk.
Vitamin C:
Foods containing vitamin C such as citrus fruits, melons, and berries help increase iron absorption.
Make sure you also check our other amazing Article on : Chronic Kidney Disease