Introduction of Arteriosclerosis:
Table of Contents
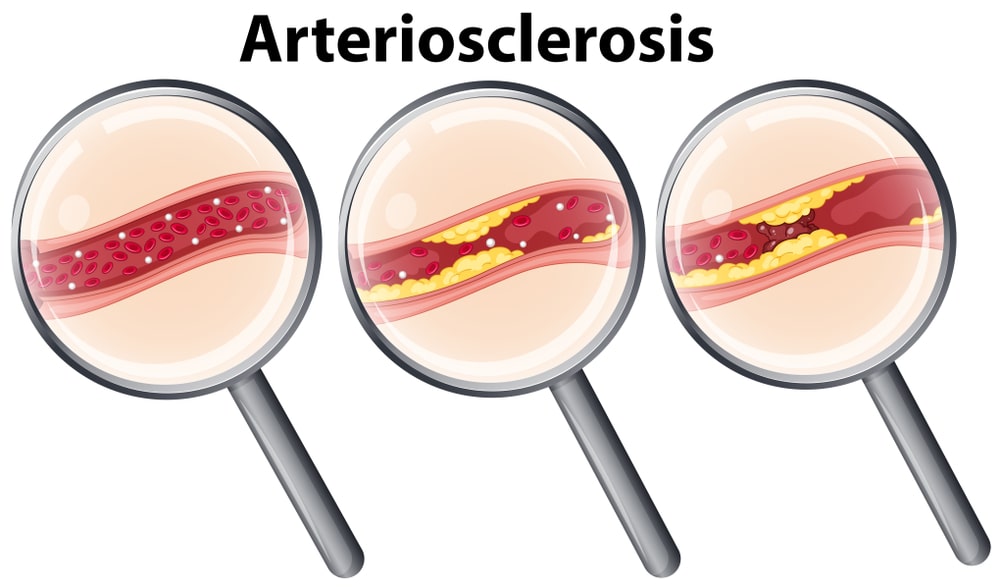
Arteriosclerosis can occur when arteries grow thick and stiff and restrict blood flow to organs and tissues in the body. This gradual process, also known as hardening of the arteries, weakens arteries and can develop in various organs, most commonly the heart.
Arteries circulate blood throughout the body, but when plaque, fat, cholesterol, and other cellular waste deposited on artery walls, arteriosclerosis can develop.
Arteriosclerosis can develop into atherosclerosis. This condition can cause heart disease, strokes, circulation problems in the arms and legs, aneurysms that can cause life-threatening internal bleeding, and chronic renal failure.
Causes of Arteriosclerosis:
Several factors can contribute to arteriosclerosis:
- High cholesterol
- High blood pressure
- Insulin resistance or diabetes
- Obesity
- Smoking or use of other tobacco products
Risk factors that contribute to arteriosclerosis include:
Family history: People with a family history of heart disease or arteriosclerosis are at higher risk for the condition.
Symptoms of Arteriosclerosis:
- Chest pain or angina.
- Pain in leg, arm, and anywhere else that has a blocked artery.
- Shortness of breath.
- Fatigue.
- Confusion, which occurs if the blockage affects circulation to the brain.
- Muscle weakness in legs from lack of circulation.
Pathophysiology of Arteriosclerosis:
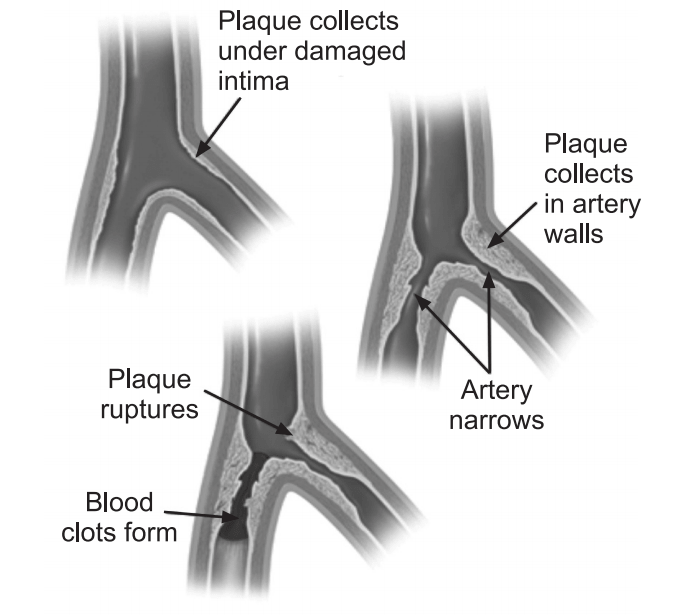
The lesions of arteriosclerosis begin as the intima (innermost layer of the blood vessel wall) of the arterial wall start to fill up with the deposition of cellular wastes. As these start to mature, they can take different forms of arteriosclerosis. All are linked through common features such as the stiffening of arterial vessels, thickening of arterial walls, and the degenerative nature of the disease.
- Arteriolosclerosis, unlike atherosclerosis, is sclerosis that only affects small arteries and arterioles, which carry important nutrients and blood to the cells.
- Atherosclerosis is the narrowing of arteries because of the deposition of plaque, usually made up of cholesterol, fatty substances, cellular waste products, calcium, and fibrin, inside the arteries. This affects large and medium-sized arteries; however, its positioning varies from person to person.
- Monckeberg’s arteriosclerosis or medial calcific sclerosis is seen mostly in old age patients, commonly in arteries of the extremities.
- Hyperplastic: Hyperplastic arteriosclerosis refers to the type of arteriosclerosis that affects large and medium-sized arteries.
- Hyaline type: Hyaline arteriosclerosis, also referred to as arterial hyalinosis and arteriolar hyalinosis refers to lesions that are caused by the deposition of homogenous hyaline in the small arteries and arterioles.
Arteriosclerosis subtypes:
Pathologically, there are two subtypes of arteriosclerosis:
- Hyperplastic type
- Hyaline type
A subclassification of arteriolosclerosis is the fibromuscular intimal thickening. There is typically hyalinosis or deposition of hyaline protein in these lesions as well. This includes the categories like:
- Transplant-related arteriopathy or arterial damage.
- Restenosis lesions are seen after balloon angioplasty or stenting of the heart’s coronary blood vessels.
- Non-specific intimal thickening occurs in temporal arteries (arteries around the forehead and temples) with aging.
Transplant arteriopathy is intimal enlargement without atherosclerotic changes seen in the walls. Transplant arteriopathy affects large and small muscular arteries and veins as well. It commonly causes inflammation in 1 or more of the 3 layers in the blood vessel walls.
Usually, the intima is affected more than the media or adventitia, but all three layers may be affected. After inflammation there is fibrosis and finally, calcification and thrombosis may occur.
Diagnosis:
Blood test:
Blood tests check the levels of certain fats, cholesterol, sugar, and protein in the blood that could indicate heart conditions.
CT scan:
X-rays and computers are used to create images of the aorta, heart, and blood vessels. This provides a more detailed picture than an ultrasound.
Electrocardiogram (EKG):
This test measures the electrical activity of the heart and can help to determine if parts of the heart are enlarged, overworked, or damaged.
Stress testing:
Used along with an EKG, the test can show changes to the heart’s rate, rhythm, or electrical activity as well as blood pressure.
Ultrasound:
An ultrasound device can measure blood pressure on various points of the arm or leg, which will help to determine any blockages and how quickly blood flows through arteries.
Treatment of Arteriosclerosis:
Treatment for arteriosclerosis includes a healthy diet, exercise, and medication to control or possibly reverse the condition. Medications to treat arteriosclerosis are based on the location of enlarged blood vessels and other underlying conditions may include.
- Cholesterol medications can protect heart arteries.
- Aspirin can prevent platelets from forming blood clots.
- β-blocker medications can reduce blood pressure and heart rate and diminish chest pains, the risk of heart attack and irregular heart rhythm.
- Angiotensin-converting enzyme (ACE) inhibitors can lower blood pressure and lower the possibility of a heart attack.
- Calcium channel blockers and diuretics (water pills) can reduce blood pressure.
- A clot-busting drug may dissolve blood clots.
Complications:
If arteriosclerosis is not diagnosed and treated, it could develop into atherosclerosis and cause serious health problems, including:
- Coronary artery disease: Narrowed arteries near the heart may lead to chest pain, heart attack, or heart failure.
- Peripheral artery disease: Narrowed arteries in the arms or legs may cause circulation problems that make it difficult to feel heat and cold, and cause gangrene that can lead to limb amputation.
- Carotid artery disease: Narrowed arteries near the brain may cause transient ischemic attack (TIA) or stroke.
- Aneurysms: A bulge in the wall of an artery, if it bursts, can cause a slow leak or life-threatening internal bleeding.
- Chronic renal failure: Narrow arteries near the kidneys can prevent effective kidney function.
Make sure you also check our other amazing Article on : Myocardial Infarction