Body Fluids and Circulation: Different types of fluids are present in different cavities in the human body. There are two types of fluids present in the human body:
- Intracellular fluid
- Extracellular fluid
1. Intracellular fluid: The fluid which is present inside cells is called intracellular fluid (ICF).
2. Extracellular fluid: The fluid which is present outside cells is called extracellular fluid (ECF). The ECF fluid which is present in small spaces between cells of tissues is known as interstitial fluid.
ECF differs depending on its location in the body:
- Blood plasma: It is the ECF within blood vessels.
- Lymph: It is the ECF present within lymphatic vessels.
- Cerebrospinal fluid: It is the ECF present in and around the brain and spinal cord.
- Synovial fluid: It is the ECF in joints.
- Aqueous humour and vitreous body: It is the ECF present in the eyes.
Cardiovascular System
Table of Contents
All cells of our body require a continuous supply of nutrients and oxygen for cellular activities. They also require a system to remove waste products formed during various activities. Most of the body cells are located at some distance from the nutrient sources such as the digestive tract and sites of waste disposal such as kidneys. The cardiovascular system plays an important role in these activities. It connects different systems in the body through a network of blood vessels and blood.
The cardiovascular system consists of:
- Blood
- The heart
- Blood vessels
Blood
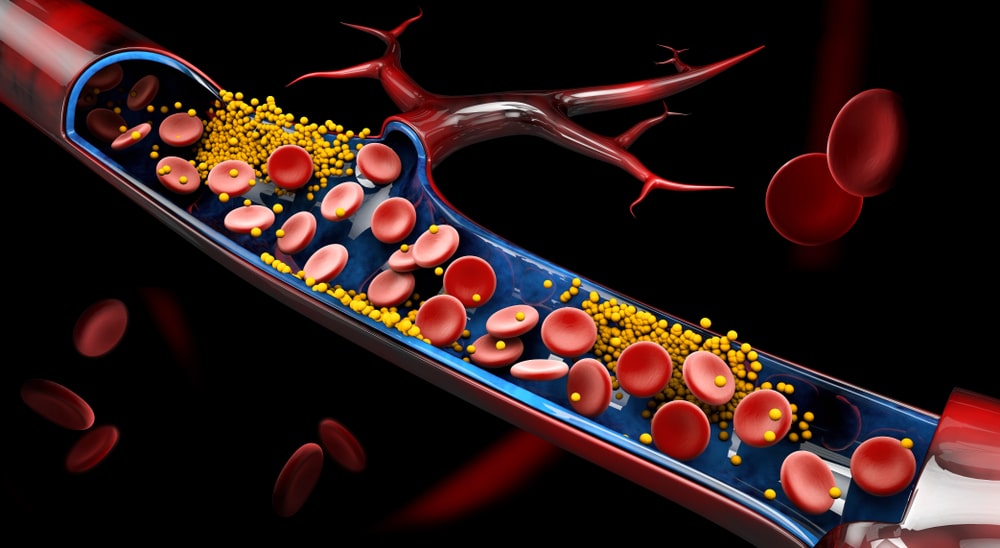
Blood is a connective tissue composed of blood plasma and different types of cells and cell fragments.
Composition of Blood:
Blood is composed of two components:
- Blood plasma
- Formed elements
1. Blood plasma:
- Blood plasma is a liquid extracellular matrix mainly consisting of water and dissolved substances.
- Blood consists of 55% blood plasma.
- Blood plasma is composed of about 91.5% water and 8.5% solutes.
- The solutes are mainly proteins (7%) and others like gases, nutrients, waste products, electrolytes (1.5%).
2. Formed elements:
- Formed elements are various types of cells and cell fragments.
- Blood contains about 45% formed elements.
- Normally, more than 99% of the formed elements are cells named for their red colour, red blood cells (RBCs).
- Pale, colourless white blood cells (WBCs) and platelets are cell fragments and occupy less than 1% of the formed elements.
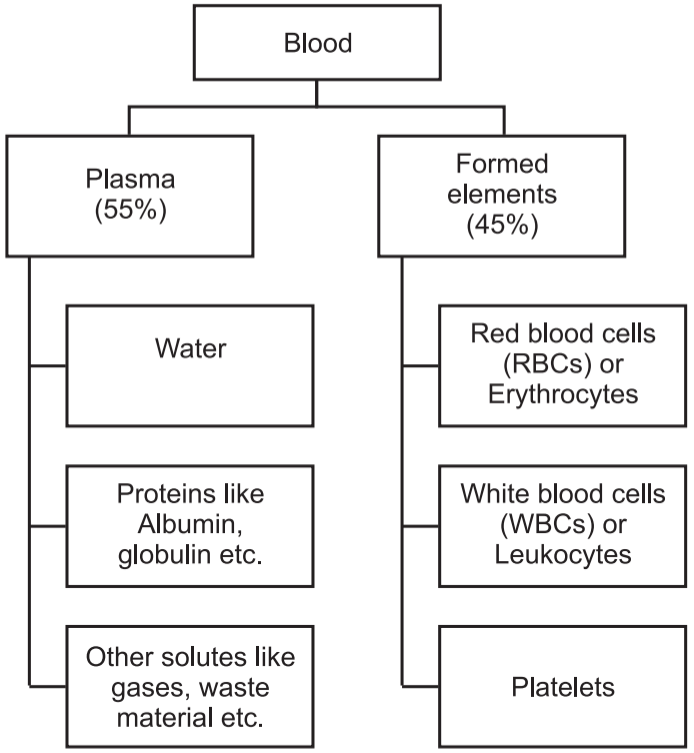
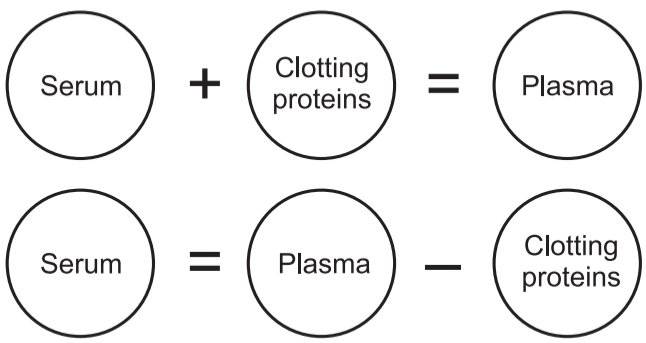
The straw-colored liquid, called serum, is part of the plasma.
Functions of Blood:
- Blood transports carbon dioxide from the body cells to the lungs and oxygen from the lungs to the cells of the body.
- Blood transfers nutrients from the gastrointestinal tract to cells.
- It transports hormones from endocrine glands to cells.
- Blood also carries heat and waste products to various organs for elimination from the body.
- Blood helps to regulate pH through the use of buffers.
- Blood also helps to adjust body temperature.
- Blood clotting protects against its excessive loss from the body after an injury.
- White blood cells protect against disease by carrying on phagocytosis.
Blood Groups:
Karl Land Steiner discovered fundamental principles of blood grouping in 1900. Blood grouping is important to avoid mismatching of blood groups as mismatching would cause hazards to the recipient. Death also may occur in mismatched blood transfusions.
The surfaces of RBCs contain a genetically determined assortment of antigens composed of glycoproteins and glycolipids. These antigens, called agglutinogens, occur in characteristic combinations. Based on the presence or absence of various antigens, blood is categorized into different blood groups. Within a given blood group, there may be two or more different blood types. There are at least 24 blood groups and more than 100 antigens that can be detected on the surface of red blood cells.
Major systems are:
- ABO system of blood grouping
- Rh system of blood grouping
(1) ABO system of blood grouping:
Blood plasma usually contains antibodies called agglutinins that react with the A or B antigens if the two are mixed. These are the anti-B antibody, which reacts with antigen A, and the anti-B antibody, which reacts with antigen B.
According to this system, there are four blood groups.
- A group – containing agglutinogen ‘A’ on cell surfaces of erythrocytes and the anti-B antibody in plasma.
- B group – agglutinogen B, the anti-A antibody.
- AB group – agglutinogens ‘A’ and ‘B’, no antibodies.
- group – No agglutinogens, anti-A antibody and the anti-B antibody.
(2) Rh blood group:
The Rh blood group is so named because the antigen was discovered in the blood of the Rhesus monkey. People whose RBCs have Rh antigens are designated Rh (Rh-positive); those who lack Rh antigens are designated Rh– (Rh-negative).
Blood Coagulation:
- In normal conditions, blood is always in liquid form when it is within blood vessels.
- When it comes out from the blood vessel, it thickens and forms a gel. In due course, the gel splits from the liquid. The gel is called a clot.
- A clot is composed of a network of insoluble protein fibres called fibrin. The process of gel formation is called clotting or coagulation.
- Blood clotting or coagulation is a series of chemical reactions that end in the development of fibrin threads.
- The process of clotting involves several elements known as clotting (coagulation) factors.
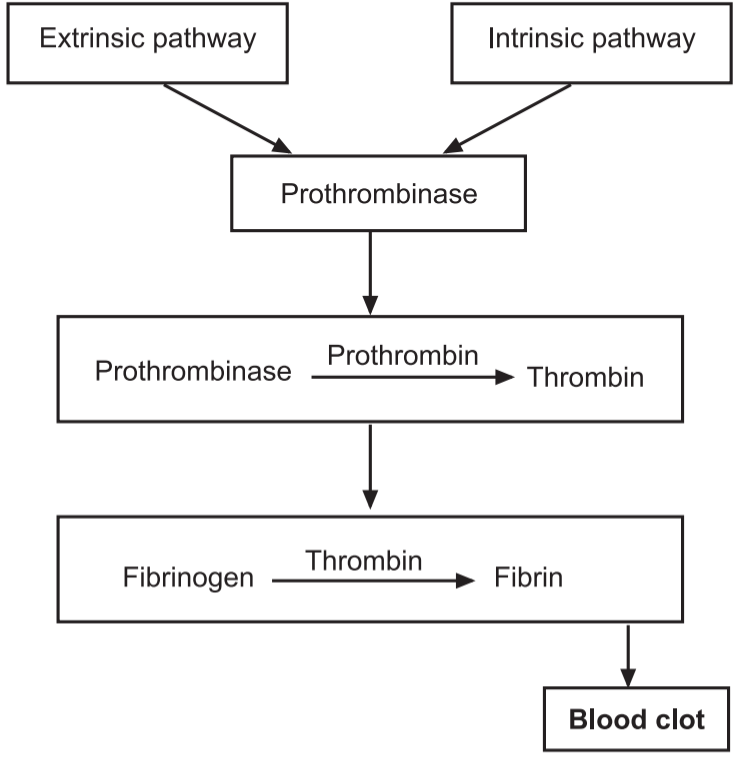
Process of Blood (Clotting) Coagulation:
Blood clotting is a complex cascade of enzymatic reactions in which each clotting factor activates many molecules of the next one in a fixed sequence. Finally, a large quantity of product (the insoluble protein fibrin) is formed.
Clotting can be divided into three stages:
- Two pathways called the extrinsic pathway and the intrinsic pathway, lead to the formation of prothrombinase.
- Once prothrombinase is formed, the steps involved in the next two stages of clotting are the same for both the extrinsic and intrinsic pathways, and together these two stages are referred to as the common pathway. Prothrombinase converts prothrombin (a plasma protein formed by the liver) into the enzyme thrombin.
- Thrombin converts soluble fibrinogen (another plasma protein formed by the liver) into insoluble fibrin. Fibrin forms the threads of the clot.
Composition and functions of Lymph:
The lymphatic system is made up of the following components:
- A fluid called lymph
- Lymphatic capillaries, Lymphatic vessels, Lymph trunk and Lymph duct
- Lymphatic organs are:
- Tonsils
- Lymph nodes
- Spleen
- Thymus
- Lymphatic tissue
- Lymphatic nodules (follicles)
- Red-bone marrow.
Functions of the Lymphatic System:
- It drains excess interstitial fluid from tissue spaces and returns it to the blood.
- It transports lipids and lipid-soluble vitamins (A, D, E and K) absorbed by the gastrointestinal tract.
- It initiates highly specific immune responses directed against particular microbes or abnormal cells.
Composition of Lymph:
- Most constituents of blood plasma filter through blood capillary walls to form interstitial fluid. After interstitial fluid passes into lymphatic vessels, it is called lymph.
- The major difference between interstitial fluid and lymph is location: Interstitial fluid is found between cells, and lymph is located within lymphatic vessels and lymphatic tissue.
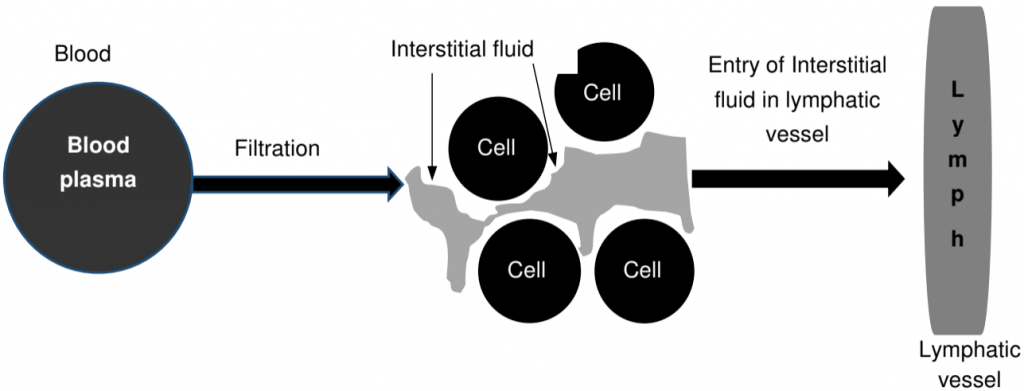
- Constituents of blood plasma like gases, nutrients and hormones, etc. filter freely through the capillary walls to form interstitial fluid.
- A considerable amount of fluid is filtered out of blood capillaries. The extra filtered fluid drains into lymphatic vessels and becomes lymph. As plasma proteins are too big to leave blood vessels, the interstitial fluid contains a lesser amount of proteins.
- The proteins can, however, move readily through the more permeable lymphatic capillaries into the lymph.
- Lymph consists of lymphocytes.
- Lymph also consists of proteins called Globulin. These are antibodies.
- Other components of the lymph plasma are very much like that of blood plasma, i.e., organic, inorganic substances, water, etc.
- An important function of lymph is to return the lost plasma proteins and plasma to the bloodstream.
Structure of Human Heart
The heart is an important organ of the cardiovascular system. It acts like a pump, which is responsible for circulating blood to all body parts. The shape of a heart is just like our closed fist. Dimensions of the heart are as follows:
- Length: 12 cm
- Width: 9 cm at its broadest point.
- Thickness: 6 cm
- Weight: 250 g in adult females and 300 g in adult males.
- Location: The heart is located in a space between two lungs of the thoracic cavity called the mediastinum. The heart is surrounded by its cavity called a pericardial cavity.
The pointed apex of the heart is directed inferiorly, and to the left and it rests on the diaphragm. The base of the heart is its posterior surface.
The sheath that surrounds and protects the heart is called the pericardium. The pericardium consists of two fused layers: an outer fibrous pericardium and an inner parietal pericardium (epicardium).
Between the pericardial sac and the heart is the pericardial cavity, which is filled with lubricating serous fluid.
The wall of the heart consists of three layers:
- The outer layer is called the epicardium.
- The middle layer is called the myocardium.
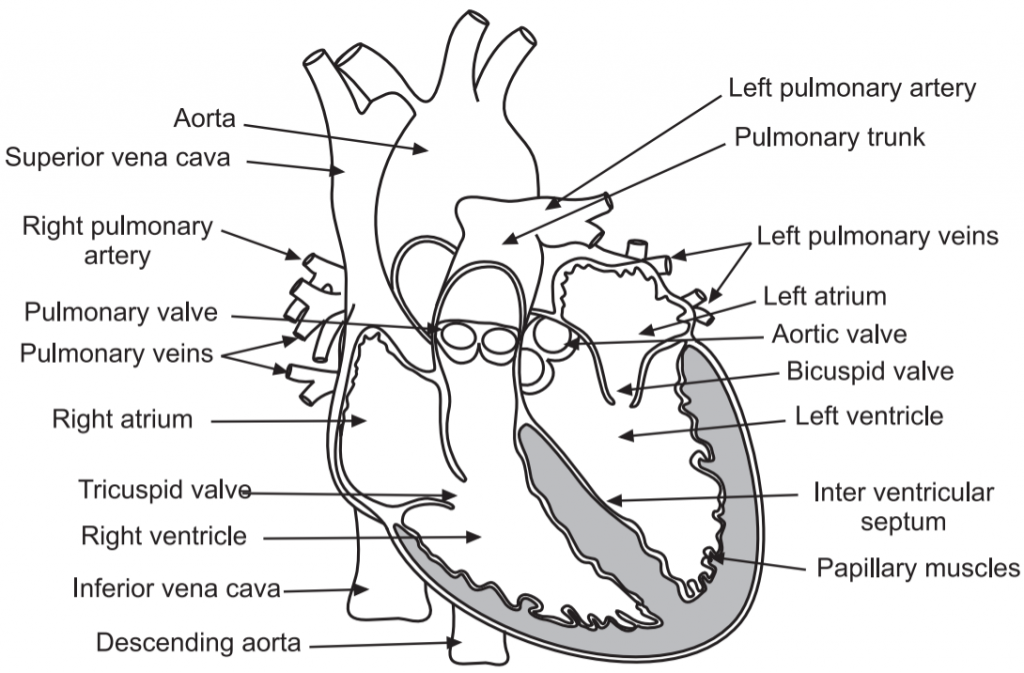
- The inner layer is called the endocardium.
- The heart is composed of four chambers: 2 atria (right atrium and left atrium) and 2 ventricles (right ventricle and left ventricle).
- Atria are receiving chambers and ventricles are pumping chambers of the heart.
- The atria receive blood from blood vessels called veins. Ventricles pump blood into blood vessels called arteries.
- The septa are the partitions that separate the chambers of the heart.
- They include the interatrial septum which separates the right and left atria.
- The interventricular septum separates the right and left ventricles.
- The right atrium is connected to the right ventricle through an opening. This opening is guarded by the atrioventricular valve called the right tricuspid valve.
- The left atrium is connected to the left ventricle through an opening. The opening is guarded by a valve called the left mitral valve.
- These valves prevent the backflow of blood. Each is attached to chordae tendineae that extend to the papillary muscles, which are extensions of the myocardium, to prevent the valves from being blown back into the atria.
- The pulmonary valve is located at the base of the pulmonary trunk, and the left semilunar valve is located at the base of the aorta.
- The right and left coronary arteries are the first to branch off the aorta and arise from two of the three sinuses located near the base of the aorta and are generally located in the sulci.
Human Circulatory System:
- The heart circulates blood in two circuits called pulmonary and systemic circulations.
- The left side of the heart is for systemic circulation and the right side is for pulmonary circulation.
- The right atrium receives systemic blood relatively low in oxygen (deoxygenated) from various body parts.
- This deoxygenation in the right atrium is transferred to the right ventricle, which pumps it into the lungs for the addition of oxygen and removal of carbon dioxide.
- Exchange of oxygen and carbon dioxide occurs in the lungs, and blood high in oxygen (oxygenated) returns to the left atrium.
- This oxygenated blood is transferred to the left ventricle, which in turn pumps it into the aorta and to all body parts.
Blood Vessels
Blood vessels have the important function of distributing blood from the heart to different tissues and also returning it to the heart.
There are five main types of blood vessels:
- Arteries
- Arterioles
- Capillaries
- Venules
- Veins
1. The blood vessels which carry blood away from the heart to other organs are called arteries. They leave the heart and divide into medium-sized, muscular arteries that branch out into the various regions of the body.
2. Medium-sized arteries then split into small arteries, which in turn split into still smaller arteries called arterioles.
3. As the arterioles enter a tissue, they branch into numerous minute vessels called capillaries.
4. Groups of capillaries within a tissue reunite to form small veins called venules.
5. These in turn merge to form progressively larger blood vessels called veins.
6. Veins are the blood vessels that convey blood from the tissues back to the heart.
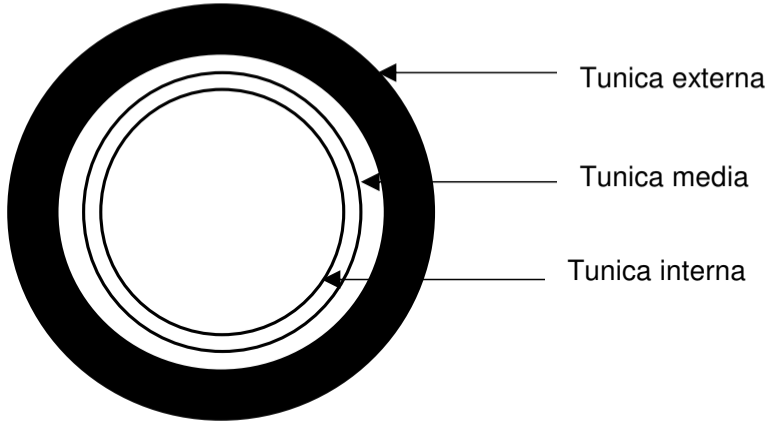
Structure:
The wall of a blood vessel consists of three layers, also called tunics.
The three structural layers are:
- The innermost layer is called tunica interna. It is made up of epithelial tissue.
- The middle layer is called tunica media. It is made up of smooth muscles.
- The outmost layer is called tunica externa. It is made up of elastic and collagen fibres.
Cardiac Cycle
- The period that begins with contraction of the atria and ends with ventricular relaxation is known as the cardiac cycle.
- The phase of contraction that the heart undergoes while it pumps blood into circulation is called systole.
- The phase of relaxation that occurs as the chambers fill with blood is called diastole.
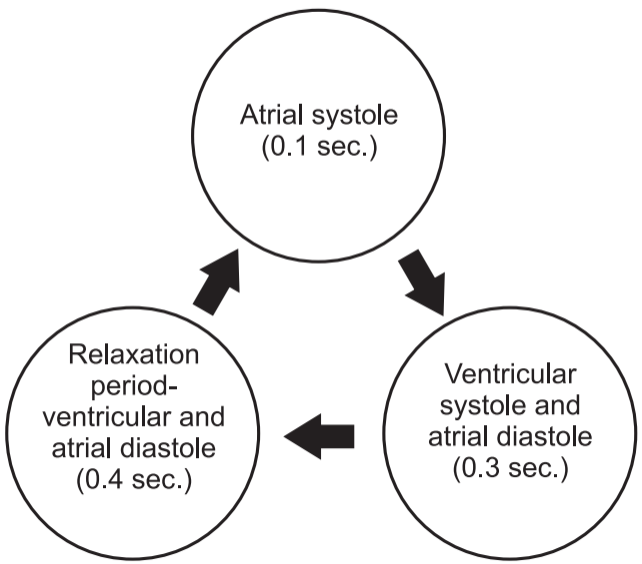
- Both the atria and ventricles undergo systole and diastole, and these components must be carefully regulated and co-ordinated to ensure blood is pumped efficiently to the body.
- In each cardiac cycle, the atria and ventricles alternately contract and relax, forcing blood from areas of higher pressure to areas of lower pressure.
- When the heart rate is 75 beats/min, a cardiac cycle lasts 0.8 sec.
Cardiac Output (CO)
Cardiac output is the volume of blood ejected from the left ventricle (or the right ventricle) into the aorta (or pulmonary trunk) each minute. Cardiac output equals the stroke volume (SV), the volume of blood ejected by the ventricle during each contraction, multiplied by the heart rate (HR), the number of heartbeats per minute:
Cardiac output = SV (ml/beat) × HR (beat/min.)
Electrocardiogram (ECG):
By careful placement of surface electrodes on the body, it is possible to record the complex, compound electrical signal of the heart. This tracing of the electrical signal is the electrocardiogram (ECG).
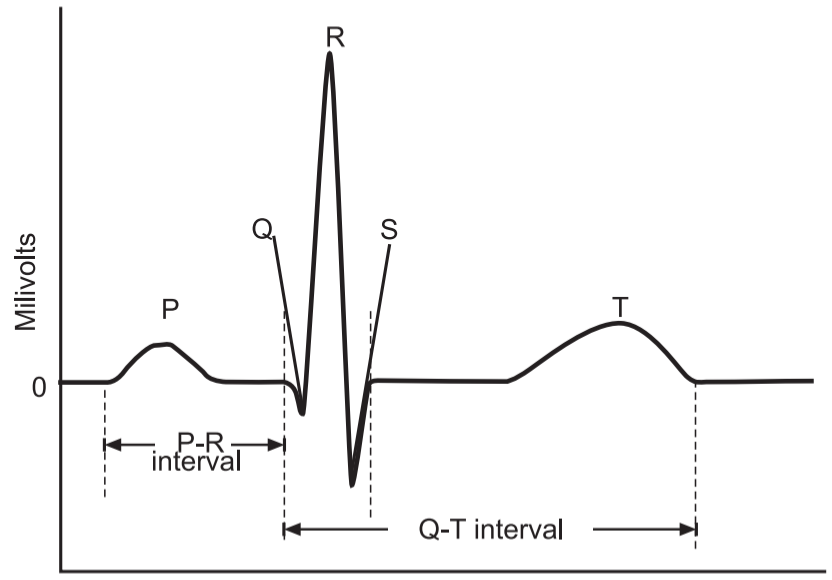
There are five prominent points on the ECG:
- The P wave,
- The QRS complex.
- The T wave.
- The small P wave represents the depolarization of the atria.
- The atria begin contracting approximately 25 ms after the start of the P wave.
- The large QRS complex represents the depolarization of the ventricles, which requires a much stronger electrical signal because of the larger size of the ventricular cardiac muscle. The ventricles begin to contract as the QRS reaches the peak of the R wave.
- Lastly, the T wave represents the repolarization of the ventricles.
- The repolarization of the atria occurs during the QRS complex, which masks it on an ECG.
Make sure you also check our other amazing article on : The Living World