Introduction of Chronic Kidney Disease:
Table of Contents
Chronic Kidney disease (CKD), also called chronic renal failure, is the irreversible loss of renal function due to the replacement of functional nephrons with fibrous scar tissue. Kidneys filter wastes and excess fluids from blood, which are then excreted in the urine. When chronic renal failure reaches an advanced stage, dangerous levels of fluid, electrolytes, and wastes can build up in the body. In the early stage of chronic renal failure, become clinically apparent as renal insufficiency, evidenced by azotemia and possibly polyurea and nocturia resulting from impaired tubular transport and concentration of urine. Chronic renal failure may not become apparent until kidney function is significantly impaired. Chronic renal failure can progress to end-stage kidney failure, which is fatal without artificial filtering (dialysis) or a kidney transplant. Chronic renal failure represents a progressive and irreversible destruction of kidney structures, leading to the accumulation of metabolic products, drugs and poisons, and disorders of water, electrolyte, acid-base balance, and renal endocrine functions.

Causes of Chronic Kidney Disease:
Chronic renal failure occurs when a disease or condition impairs kidney function, causing kidney damage to worsen over several months or years.
Diseases and conditions that commonly cause chronic renal failure include:
- Type 1 or type 2 diabetes,
- High blood pressure.
One of the complications resulting from diabetes or high blood pressure is the damage to the small blood vessels in the body. The blood vessels in the kidneys also become damaged, resulting in CKD.
The most common cause of end-stage renal failure worldwide is IgA nephropathy (Inflammation in the kidney).
Other common causes of chronic renal failure include
- Recurring pyelonephritis (kidney infection).
- Polycystic kidney disease (multiple cysts in the kidneys), Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate, kidney stones, and some cancers.
- Autoimmune disorders such as systemic lupus erythematosus.
- Hardening of the arteries, which can damage blood vessels in the kidney.
- Urinary tract blockages and reflux, due to frequent infections, stones, or an anatomical abnormality that happened at birth.
- Excessive use of medications that are excreted through the kidneys.
- Vesicoureteral reflux, a condition that causes urine to back up into the kidneys.
Pathophysiology of Chronic Kidney Disease:
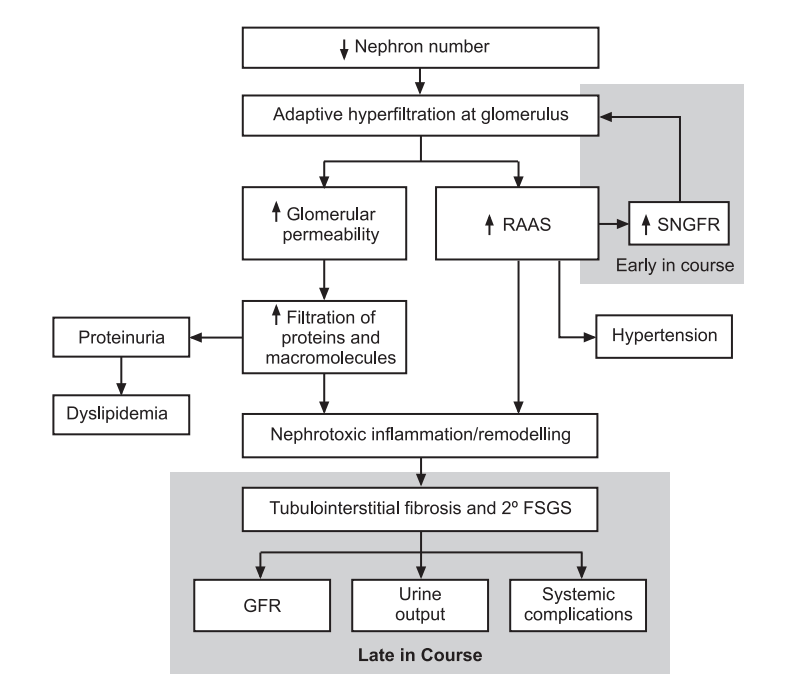
A normal kidney contains approximately 1 million nephrons, each of which contributes to the total glomerular filtration rate (GFR). In the face of renal injury (regardless of the etiology), the kidney has an innate ability to maintain GFR, despite progressive destruction of nephrons, as the remaining healthy nephrons manifest hyperfiltration and compensatory hypertrophy. This nephron adaptability allows for continued normal clearance of plasma solutes. Plasma levels of substances such as urea and creatinine start to show measurable increase only after total GFR has decreased to 50%
The plasma creatinine value will approximately double with a 50% reduction in GFR. For example, a rise in plasma creatinine from a baseline value of 0.6 mg/dL to 1.2 mg/dL in a patient, although still within the adult reference range, actually represents a loss of 50% of functioning nephron mass.
The increased glomerular capillary pressure may damage the capillaries, leading initially to secondary focal and segmental glomerulosclerosis (FSGS) and eventually to global glomerulosclerosis.
Symptoms of Chronic Kidney Disease:
Signs and symptoms of chronic renal failure develop over time if kidney damage progresses slowly. Signs and symptoms of chronic renal failure may include:
- Nausea,
- Vomiting,
- Loss of appetite,
- Fatigue and weakness,
- Sleep problems,
- Changes in urine output,
- Decreased mental sharpness,
- Muscle twitches and cramps,
- Hiccups,
- Swelling of feet and ankles,
- Persistent itching,
- Chest pain, if fluid builds up around the lining of the heart,
- Shortness of breath, if fluid builds up in the lungs,
- High blood pressure (hypertension). Signs and symptoms of kidney disease are often nonspecific; they can also be caused by other illnesses. Because kidneys are highly adaptable and able to compensate for lost function, signs and symptoms may not appear until irreversible damage has occurred.
Table: Mechanisms of nephropathy in renal failure
| Mechanism | Description |
| Glomerulosderosis | Progressive, destructive hardening of glomerular capillaries initiated by adaptive changes in the nephrons, which are initially unaffected by a primary disease process. Epithelial and endothelial injury results in proteinuria. Hardening is due to mesangial cell proliferation, increased production of extracellular matrix, and intraglomerular coagulation. |
| Tubulointerstitial injury | Defects in tubular transport function associated with interstitial edema, leukocyte infiltration, and focal tubular necrosis. |
| Vascular injury | Diffuse or focal ischemia of the renal parenchyma is associated with thickening, fibrosis, or focal lesions of renal blood vessels. Reduced blood flow may result in tubular atrophy and interstitial fibrosis as well as functional disruption (e.g., reduced glomerular filtration rate, proteinuria, and alteration of the medullary gradient with loss of concentrating ability). |
Tests and Diagnosis of Chronic Kidney Disease:
Blood tests:
Kidney function tests look for the level of waste products, such as creatinine and urea in the blood. Higher levels of creatinine indicate a lower glomerular filtration rate and as a result a decreased capability of the kidneys to excrete waste products.
Urine tests:
Testing of a urine sample shows that the kidney is allowing the loss of protein or red blood cells into the urine. It may reveal abnormalities that point to chronic kidney failure and help to identify the cause of chronic renal failure.
Treatments of Chronic Kidney Disease:
There are two treatments for kidney failure:
1. Dialysis.
2. Kidney transplantation
1. Dialysis:
Two different types of dialysis can be done.
- Hemodialysis (HD).
- Peritoneal Dialysis (PD).
Hemodialysis Purpose:
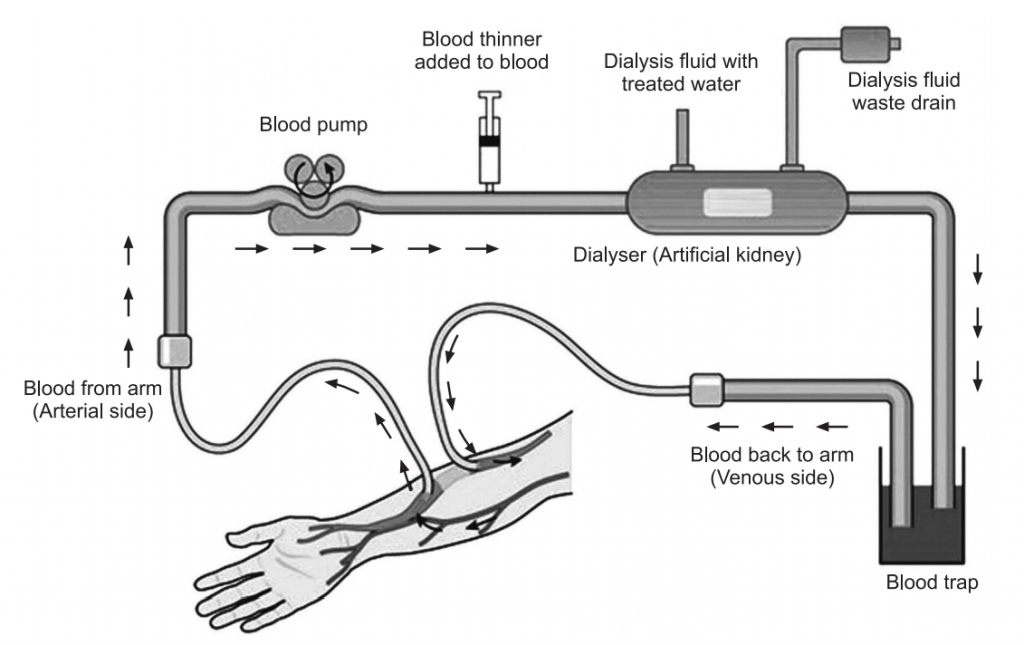
Hemodialysis cleans and filters blood using a machine to temporarily rid the body of harmful wastes, extra salt, and extra water. Hemodialysis helps to control blood pressure and helps the body to keep the proper balance of important chemicals such as potassium, sodium, calcium, and bicarbonate.
Dialysis can replace part of the function of the kidneys. Diet, medications, and fluid limits are often needed as well. Diet, fluids, and the number of medications needed will depend on treatment.
Hemodialysis Working:
Hemodialysis uses a special filter called a dialyzer that functions as an artificial kidney to clean blood. The dialyzer is a canister connected to the hemodialysis machine.
During treatment, blood travels through tubes into the dialyzer, which filters out wastes, extra salt, and extra water. Then the cleaned blood flows through another set of tubes back into the body. The hemodialysis machine monitors blood flow and removes wastes from the dialyzer.
Peritoneal Dialysis:
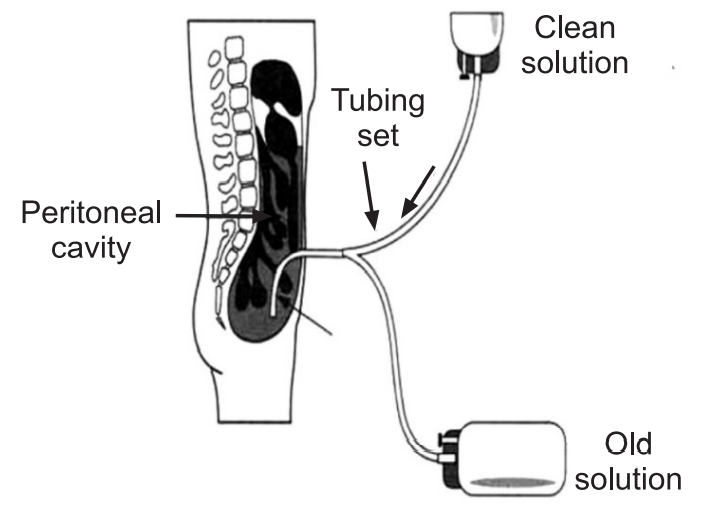
Peritoneal dialysis is another procedure that removes wastes, chemicals, and extra water from the body. This type of dialysis uses the lining of the abdomen, or belly, to filter blood. This lining is called the peritoneal membrane and acts as the artificial kidney.
Peritoneal Dialysis Working:
A mixture of minerals and sugar dissolved in water, called dialysis solution, travels through a catheter into the belly. The sugar (dextrose) draws wastes, chemicals, and extra water from the tiny blood vessels in the peritoneal membrane into the dialysis solution. After several hours, the used solution is drained from the abdomen through the tube, taking the wastes from blood with it. Then abdomen is refilled with fresh dialysis solution, and the cycle is repeated. The process of draining and refilling is called an exchange.
Dialysis is not a cure:
Hemodialysis and peritoneal dialysis are treatments that help to replace the work kidneys did. These treatments help to feel better and live longer, but they do not cure kidney failure. Although patients with kidney failure may live longer than ever, over the years kidney disease can cause problems such as heart disease, bone disease, arthritis, nerve damage, infertility, and malnutrition.
2. Kidney Transplant:
A kidney transplant involves surgically placing a healthy kidney from a donor into the body. The transplanted patient may need to take medications for the rest of their life to keep the body from rejecting the new organ.
Treatments and Drugs of Chronic Kidney Disease:
Chronic renal failure has no cure. In general, treatment consists of measures to help control signs and symptoms, reduce complications, and slow the progression of the disease. If kidneys become severely damaged, may need treatment for end-stage kidney disease.
Treating Complications:
Kidney disease complications can be controlled to make them more comfortable. Treatments may include:
High blood pressure medications:
People with kidney disease may experience worsening high blood pressure. Recommend medications to lower blood pressure, commonly angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers, and to preserve kidney function. High blood pressure medications can initially decrease kidney function and change electrolyte levels, may need frequent blood tests to monitor the condition.
Medications to lower cholesterol levels:
Medications (statins) are used to lower cholesterol. People with chronic renal failure often experience high levels of bad cholesterol, which can increase the risk of heart disease.
Medications to treat anemia:
In certain situations, may recommend supplements of the hormone erythropoietin, sometimes with added iron. Erythropoietin supplements aid in the production of more red blood cells, which may relieve fatigue and weakness associated with anemia.
Medications to relieve swelling:
People with Chronic renal failure may retain fluids. This can lead to swelling in the legs, as well as high blood pressure. Diuretics can help maintain the balance of fluids in the body.
Medications to protect bones:
Calcium and vitamin D supplements may be useful to prevent weak bones and lower the risk of fracture.
Table: Levels of treatment in CRF
| Treatment Mode | Description |
| Conservative Treatment: Protein restriction Tight glycemic control (in diabetics) | Protein intake restricted to 0.6-0.8 g/day. Frequent glucose testing with appropriate dose insulin, divided-oral hypoglycemic therapy, or dietary measures. |
| Angiotensin-converting enzyme inhibitors (e.g., captopril) | Drug therapy to interrupt the renin-angiotensin-aldosterone system, improving renal blood flow and protecting against hypertensive nephropathy. |
| Diuretics Erythropoietin | Drug therapy to augment sodium and water excretion. Use of recombinant erythropoietin to treat anemia due to defective production of this hormone in renal disease. |
| Low phosphate diet, calcium supplementation, vitamin D | Prevention and treatment of renal osteodystrophy. |
| Renal Replacement Therapy: Hemodialysis | Use of an extracorporeal circuit to create a blood flow rate of 200-400 mL/min through an artificial kidney (dialyzer). The patient’s blood flows countercurrent to dialysate fluid, with the exchange of water and solutes to affect normal fluid and electrolyte balance. |
| Peritoneal dialysis | Use of the peritoneal membrane for exchange of water and solute between patient’s blood (in the abdominal wall and visceral capillaries) and dialysate instilled into the peritoneal cavity. |
Make sure you also check our other amazing Article on : Acute Renal Failure