DEFINITION
Table of Contents
Congestive heart failure (CHF) is a clinical syndrome during which the center is unable to pump ample blood to fulfill the metabolic necessities of the body, or will do this solely at an elevated filling pressure.
EPIDEMIOLOGY
- Heart failure may be a burgeoning downside worldwide, with over twenty million folks affected.
- The overall prevalence of HF within the adult population in developed countries is 2%.
- HF prevalence follows an exponential pattern, rising with age, and affects 6-10% of people over age 65.
- The incidence of HF is lower in women than in men.
- Although HF once was thought to arise primarily within the setting of a depressed left chamber (LV) ejection fraction (EF), medical specialty studies have shown that around a simple fraction of patients WHO develop HF have a standard or preserved EF (EF 40-50%).
- Accordingly, HF patients are now broadly categorized into one of two groups: (1) HF with a depressed EF (systolic failure) or (2) HF with a preserved EF (diastolic failure).
CLASSIFICATION OF CHF
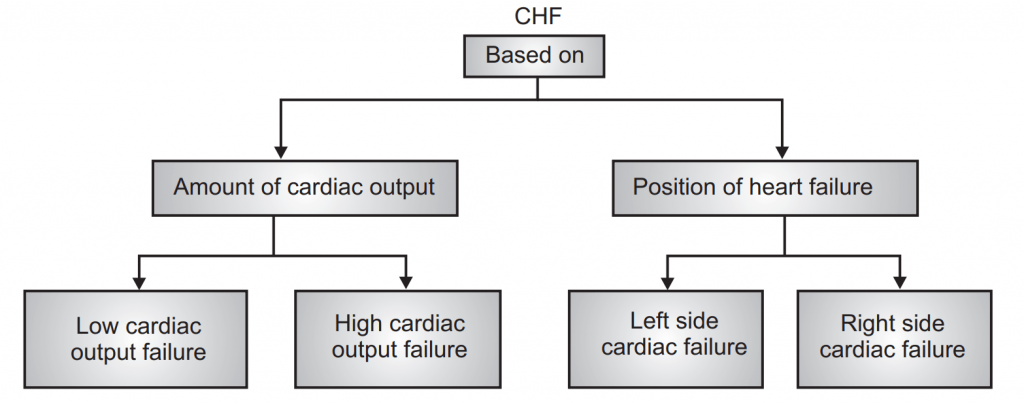
Based on the amount of Cardiac Output:
| Low cardiac Output Failure | High cardiac Output Failure |
| Most frequent. | Very rarely. |
| Metabolic demands of the body organs for oxygen are normal and within limits. | The metabolic demands of the body for oxygen are very high. |
| Myocardial fraction is a prominent factor leading to the failure of systolic and diastolic function of the ventricles, ultimately results in low cardiac output failure. | Hyperthyroidism, anemia, arteriovenous shunt causes high cardiac output failure. |
Based on the position of Heart Failure:
| Left side Cardiac Failure | Right side Cardiac Failure |
| Is the result of right-side cardiac failure. | Is the result of left side cardiac failure |
| The inefficient pumping action of the left ventricle is responsible for the accumulation of blood in the ventricles. | The inefficient pumping action of the right ventricle is responsible for the accumulation of blood in the right ventricle. |
| The left ventricle fails to accept/collect the blood from the lungs due to backpressure. | The right ventricle fails to accept/collect the blood from peripheral organs. |
| Pulmonary congestion/edema is the final result. | Peripheral generalized edema is the final result. |
PATHOPHYSIOLOGY OF CONGESTIVE CARDIAC FAILURE (C.C.F)
The cardiac membrane is lipoproteins in nature. Normally Na+ ions are concentrated extracellularly.
When Na+ levels fall ↓ The sarcoplasmic reticulum remains inactive ↓ Causes low level of Ca++ ↓ This leads to weak myocardial systole ↓ This causes accumulation of blood in ventricles ↓ This leads to ventricular distension ↓ The heart tries to expel this accumulated blood volume ↓ Gets exhausted and fails to work ↓ This failed due to the accumulation of blood volume is defined as ↓ Congestive Heart Failure
Compensatory Mechanisms of CHF
To enhances the cardiac output, the body compensates for the intrinsic cardiac effects in the following manner.
1. Increased sympathetic discharge.
2. To complete the remittent B.P., baroreceptors set within the arch of artery arterial blood vessel sinuses and walls of the center get excited and cause activation of beta-adrenergic receptors increasing rate and force of contraction of the heart.
3. An increase in blood vessels comes back (preload) is additionally seen because of the activation of alpha-adrenergic receptors.
4. Increased rate associated force of contraction at the side of the enhanced preload ends up in an initial increase within the flow.
5. Vasoconstriction of the arteries due to alpha stimulation also causes an increase in afterload, leading to falling in ejection fraction.
Activation of Renin Angiotensin Aldosterone (RAA)
- Fall within the flow decreases the urinary organ perfusion rate; as a result, the RAA system gets activated.
- Angiotensin II may cause an atrophic response in vascular smooth muscle (with vasoconstriction) and myocardial hypertrophy, attempting to restore wall stress to normal.
Cardiac Remodeling:
It is a most vital mechanism by that body stipendiary for the intrinsic internal organ effects.
- It involves changes within the form of the center (from traditional to spherical) because of cardiac muscle hypertrophy.
- During cardiac remodeling, the connective tissue cells as well as the abnormal myocardial cells undergo proliferation and dilation instead of stretching under the influences of angiotensin-2.
- In the early stages, the remodeled heart maintains cardiac performance.
- But later on, hypertrophy may exert certain adverse effects like ischaemic changes, decrease in the rate and force of contraction of the heart. After a certain time, the antagonistic mechanisms get exhausted and worsen the cardiac performances. The stress on the heart increases and a stage is reached where these mechanisms fail to maintain adequate cardiac output.
Clinical manifestations/signs and symptoms
- Fluid retention
- Pulmonary congestion
- Dyspnoea and orthopnoea
CVS Manifestations
- Resting tachycardia
- Ventricular arrhythmias
- Enlargement of heart
Renal Manifestations
- Nocturia
- Oliguria
Other Manifestations
- Reduced cardiac output leads to poor perfusion of skeletal muscle resulting in fatigue.
- The reduced flow results in poor perfusion of muscle leading to fatigue.
- Reduced perfusion to the brain results in altered mental states and confusion.
- Reduced perfusion might also cause the patient to seem pale with cold and perspiring hands.
Treatment
Non-drug treatment/ non pharmacological approach:
- Physical exercise
- Salt intake
- Fluid intake
- Alcohol consumption
- Licorice
DRUG THERAPY
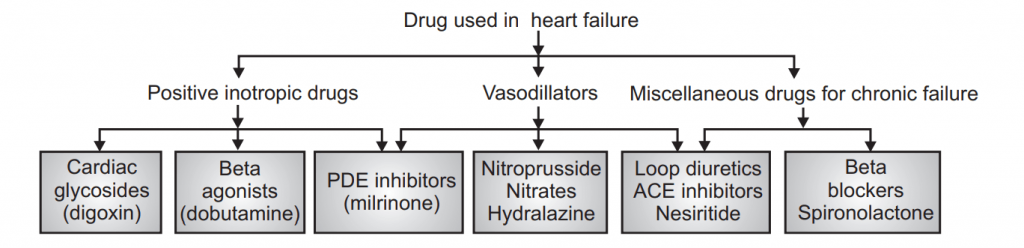
Inotropes:
- Increase the force of contraction.
- All increase intracellular cardiac Ca++ concentration.
E.g. Digitalis (cardiac glycoside), Dobutamine (β-adrenergic receptor agonist), Milrinone.
Non-pharmacological Approaches:
CARDIAC GLYCOSIDES
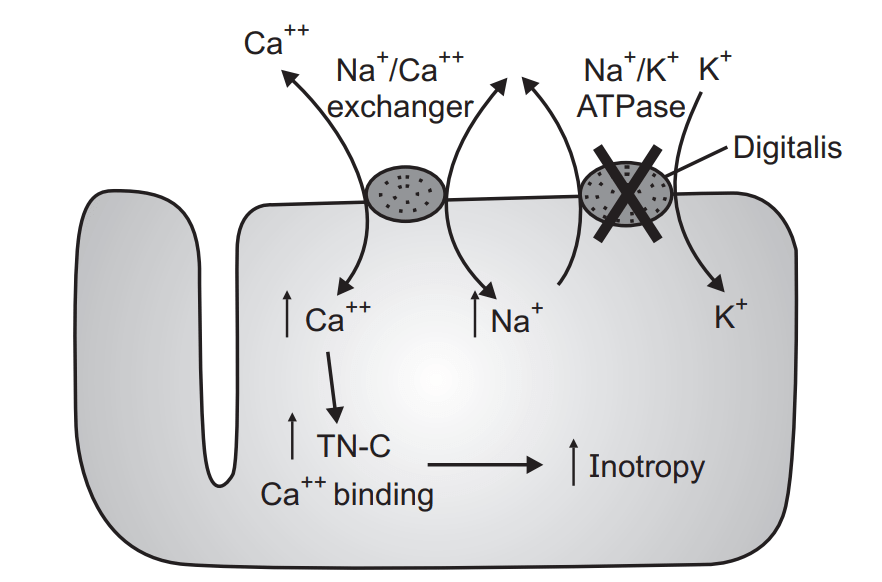
Mechanism of action:
“Effect on cardiovascular function in CHF”.
1. Digitalis derivatives when administrated to individuals suffering from CHF:
- Acts directly on the myocardium and increases conductivity, automaticity, rhythmicity, and causes forceful contraction of the heart. Because of powerful contractions, ventricular blood is forced from the right side into the artery and from the left ventricles to the aorta. This causes complete emptying of the heart.
- Digitalis derivatives block Na+ – K+ ATPase enzymes and improve the level of Na+ and act as represented below:
Digitalis ↓ Blocks Na+ - K+ ATPase enzyme ↓ Increases Na+ plasma level ↓ Activates sarcoplasmic reticulum ↓ Releases Ca++ ↓ Combines with cardiac muscles ↓ Causes forceful contraction ↓ This leads to complete emptying of the heart (ventricles) ↓ Thus relieves congestion ↓ Restore myocardial function
Thus digitalis derivatives, by their direct and indirect action, improve the force of contractility and thereby assure complete emptying of the heart. Thus digitalized hearts can do work with less energy expenditure or more work with some energy expenditure. Hence, digitalis is defined as “Cardiotonic”.
2. Effect on automaticity, conductivity, contractility, blood pressure, heart rate:
- Automaticity: Digitalis increases the ability of Purkinje cells and ventricular muscles to initiate impulses.
- Conduction velocity: The conduction velocity is slightly increased in the atria and ventricle by small doses of digitalis.
- Blood pressure: Digitalis increases mean arterial pressure in normal individuals only.
- Heart rate: Digitalis does not affect heart rate in normal individuals, but reduces it in CHF patients.
Extra Cardiac Actions:
- On kidney: Digitalis increases the rate of excretion of Na+ and water by the kidney and thus exerts diuresis.
- On Gastro-intestinal Tract: High doses of digitalis produce diarrhea, nausea, vomiting.
Side Effects:
- Anorexia, nausea, vomiting, diarrhea.
- Headache, fatigue, insomnia.
- Yellow/green vision, blurred vision.
- Cardiac arrhythmia.
Therapeutic Uses:
- To treat heart failure.
- To treat atrial fibrillation.
- To treat atrial flutter.
- To treat paroxysmal atrial tachycardia.
Contraindication:
Digitalis is strictly contraindicated in the following clinical conditions:
- Myocardial infarction
- Ventricular tachycardia
- Partial heart block
- Previous digitalis therapy
- Calcium administration.
Digitalis interaction:
- Digitalis, Calcium: Calcium ions increase the force of contraction of the heart. High plasma calcium levels stimulate the myocardium so much, that it leads to cardiac arrest during systole. Digitalis is also known to increase the force of contraction of the heart. Thus digitalis and calcium act synergetically and may prove to be toxic. Hence during digitalis therapy, Ca++ ion administration must be avoided.
- Digitalis, Quinidine: Quinidine, when administrated in individuals taking digitalis, increases serum digoxin levels. This may cause adverse effects of digitalis and other clinical complexities. Hence must be avoided.
Treatment of over digitalization:
- Immediately stop the administration of digitalis.
- Stop if any diuretic administration is in continuation.
- Mild tachycardia can be treated with atropine.
- Mild toxicity can be treated by administration of potassium salts – 5 to 7.5 g of potassium chloride orally daily.
- Ventricular tachycardia can be treated with phenytoin (250 mg well diluted).
Rapidly Acting Inotropic Agents
In critically sick infants with CHF, in those with renal dysfunction (e.g., infants or in postoperative cardiac patients with heart failure) quickly acting catecholamines with a short duration of action is preferable to digoxin.
- dopamine,
- dobutamine
- epinephrine
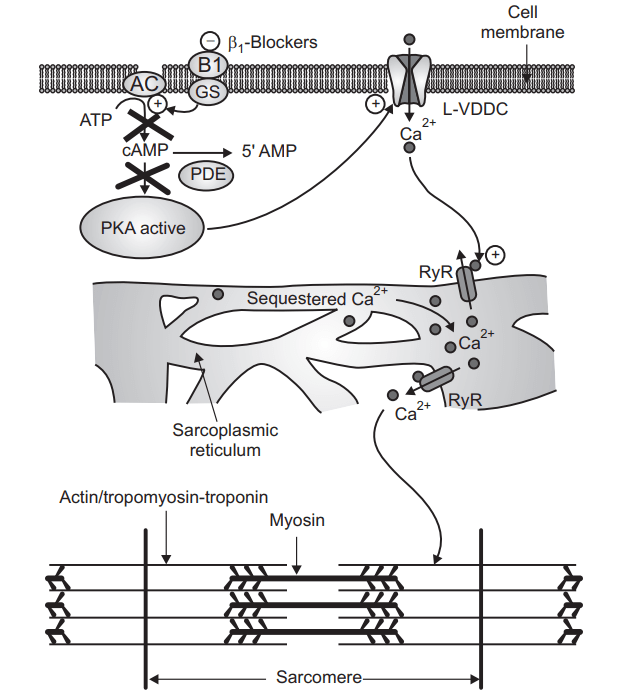
β1 Blockers:
β1-Blockers-bisoprolol, carvedilol, metoprolol.
Mechanism of Action:
- Heart failure is accompanied by increased activation of the sympathetic nervous system.
- This brings about structural and functional modification in the myocardium.
- β Blockers inhibit the sympathetic outflow of norepinephrine and counteract the changes produced.
- The ventricular remodeling in heart failure is also reversed by β Blockers.
- Increases beta-receptor sensitivity.
Adverse drug reaction:
- Hypotension
- Bradycardia.
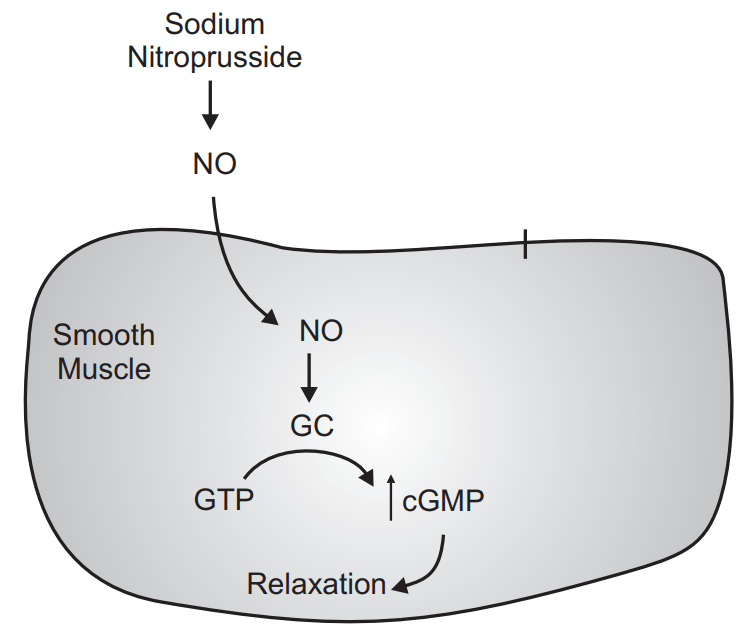
VASODILATORS
- Isosorbide dinitrate, isosorbide mononitrate, and hydralazine are also used especially in patients who cannot tolerate ACE inhibitors.
Mechanism of Action:
• It directly relaxes the arterioles and arteries reducing the peripheral vascular resistances, preload and help to reduce
afterload.
Adverse drug reaction:
- Nausea
- Palpitation
- Tachycardia
- Salt and water retention on prolong therapy.
ACE INHIBITORS
- Captopril, Enalapril, Fosinopril, Lisinopril, Ramipril, Quinapril.
Mode of action:
- They inhibit the generation of angiotensin 2, a potent vasoconstrictor.
- They also inhibit the release of aldosterone and vasopressin, thereby inhibiting fluid and slat retention thus decreasing the preload.
- Elevate the levels of bradykinin.
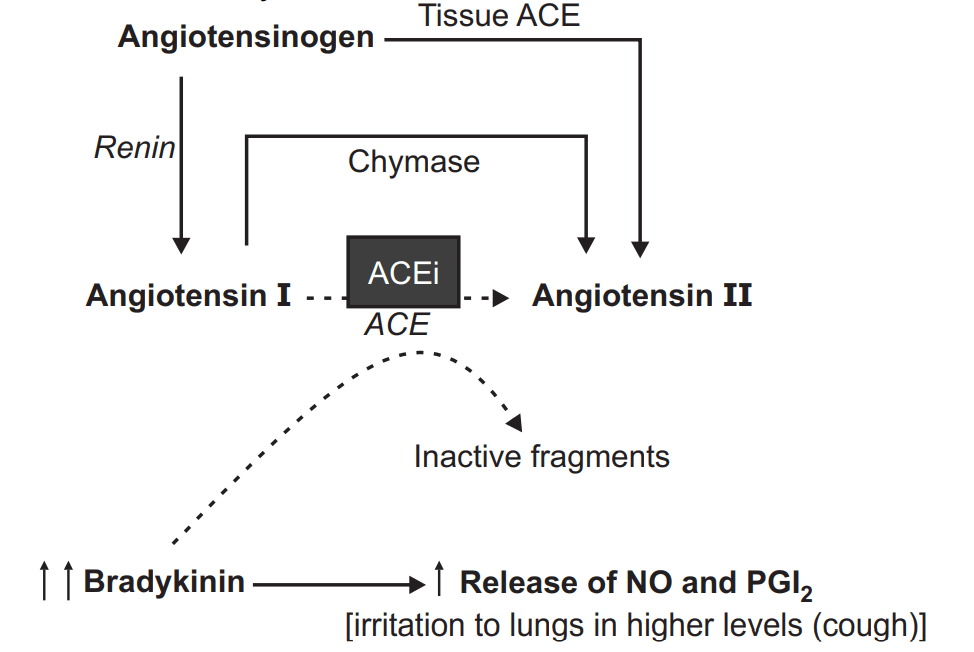
Adverse drug reaction:
Postural hypotension, hyperkalemia, dry cough.
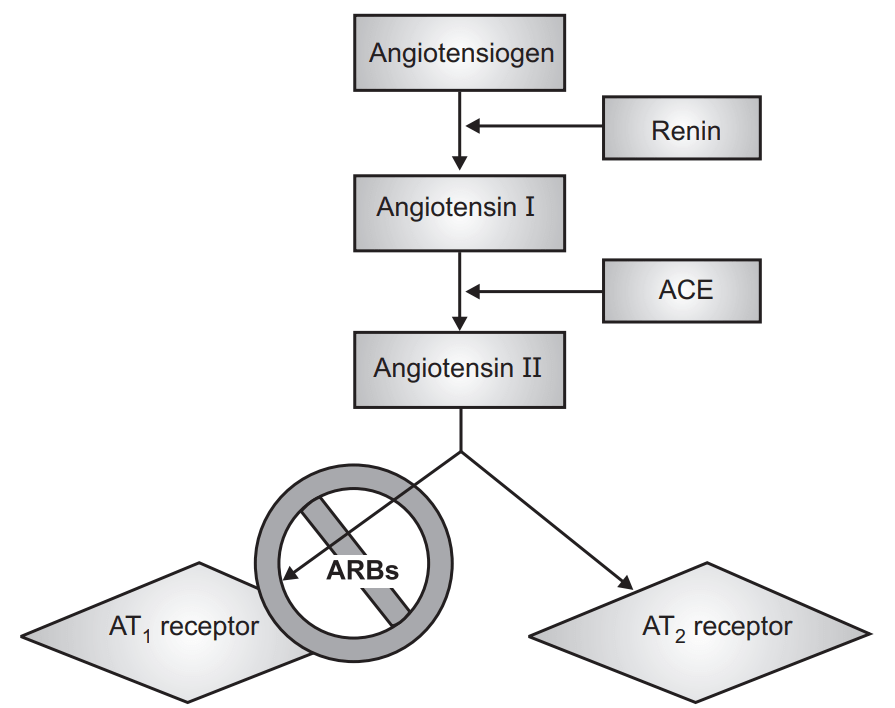
Angiotensin Receptor AT-1 blockers (ARB).
Losartan, Candesartan, Valsartan, Telmisartan.
Mode of Action:
- Angiotensin-2, a vasoconstrictor is concerned with ventricular remodeling and fluid retention.
- These drugs inhibit the binding of angiotensin 2 to its AT₁ receptor.
- Thus they preclude the above-mentioned effects of angiotensin 2.
- These agents do not exert any action on bradykinin and thus do not produce cough.
- Has a comparable effect to ACE I.
- Can be used in certain conditions when ACE I are contraindicated.
Adverse drug reactions:
- Orthostatic Hypotension.
- Hyperkalemia
- Headache
- Dizziness
- Impairment of renal functioning.
DIURETICS
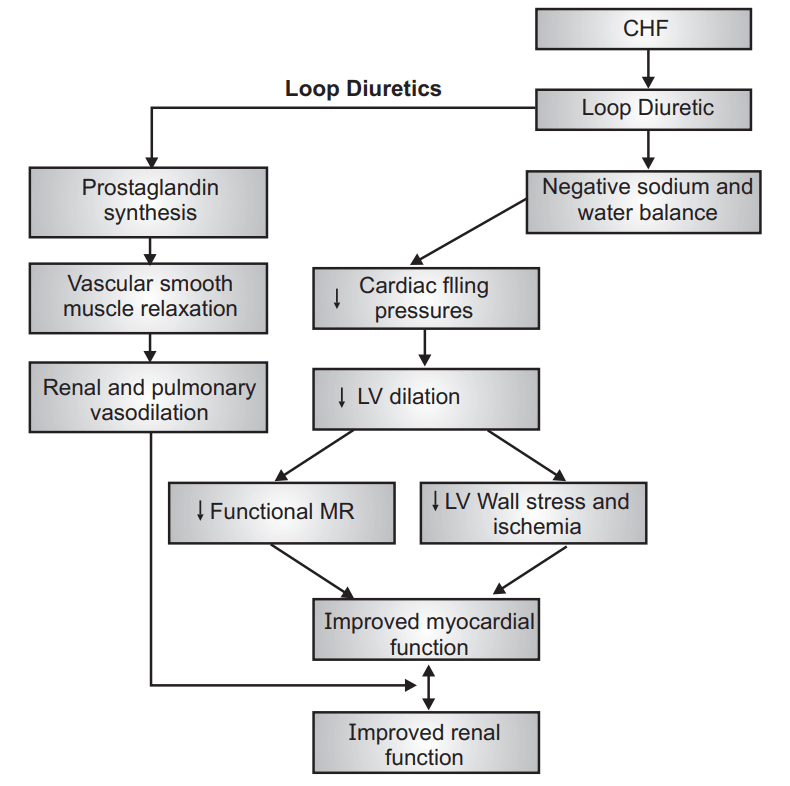
- Bumetanide, Furosemide, Metolazone, Torsemide.
- Diuretics remain the principal therapeutic agent to control pulmonary and systemic venous congestion.
- Diuretics reduce preload and improves congestive symptoms, but do not improve cardiac output or myocardial contractility.
- Loop diuretics commonly used.
- Aldosterone antagonists – used in conjunction with a loop diuretic.
Make sure you also check our other amazing Article on : Gonorrhoea