Diuretics
Diuretics are the materials that promote the excretion of urine.
- Promotes the excretion of the (Na+ ), (Cl– ), or (HCO-3) and water.
- The net result being:
- Increase the urine flow.
- Change urine pH.
- Change the ionic composition of the urine and blood.
- Diuretics are very effective in treating edema, CHF, pregnancy, nutritional nephrotic syndrome, hypertension, cirrhosis of the liver, and lower intracellular and CSF pressure.
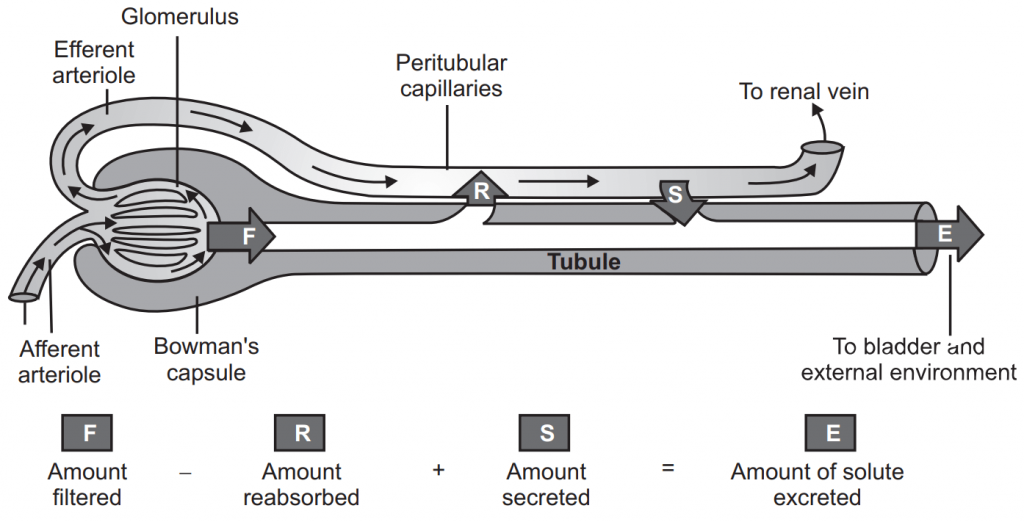
Normal Physiology of Urine Formation
- Kidney: 1.3 million nephrons each.
- Glomerular Filtration:
- Receive 25% of cardiac output
- Filtration rate: 100-120 ml/minute
- 180 L of glomerular filtrate/day.
- Tubular Reabsorption:
- Reabsorption of 99% of glomerular filtrate
- 1.5 L/day of urine.
- Tubular Secretion:
Classification of Diuretics
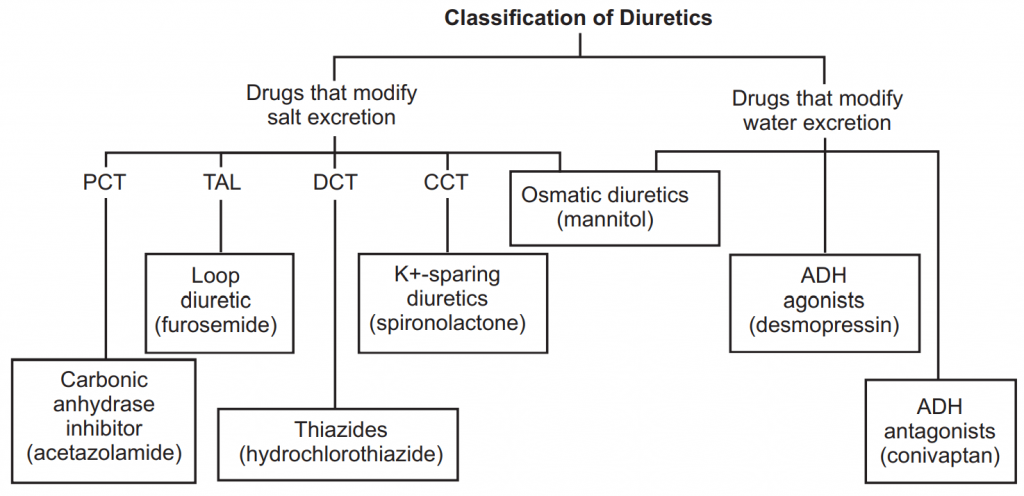
Proximal Convoluted Tubule (PCT), Thick Ascending Limb of the loop of Henle (TAL), Distal Convoluted Tubule (DCT), and Cortical Collecting Tubule (CCT).
Site And Mechanisms of Actions of Diuretics
| Diuretics | Site of Action | Mechanism |
| Osmotic Diuretic | 1. Proximal tubules 2. Loop of Henle 3. Collecting duct | Inhibition of water and Na+ reabsorption. |
| Carbonic Anhydrase Inhibitor (CA-I) | Proximal tubules | Inhibition of bicarbonate reabsorption. |
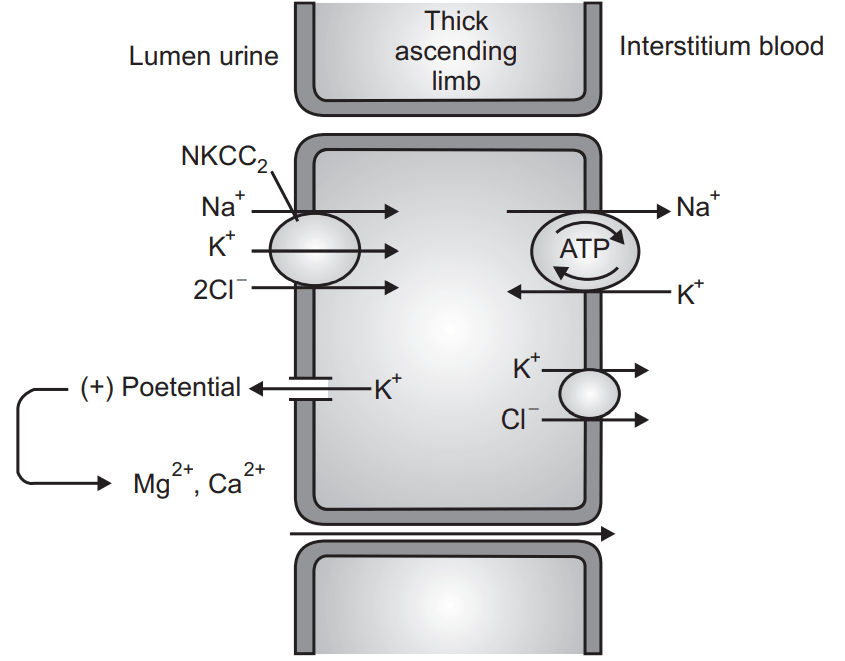
| Loop Diuretic | Loop of Henle (thick ascending limb) | Inhibition of Na+ , K+ , Cl cotransport. |
| Thiazide | Early distal tubule | Inhibition of Na+, Cl cotransport |
| K+ sparing diuretics | Late distal tubule Collecting duct | Inhibition of Na+ reabsorption and K+ secretion. |
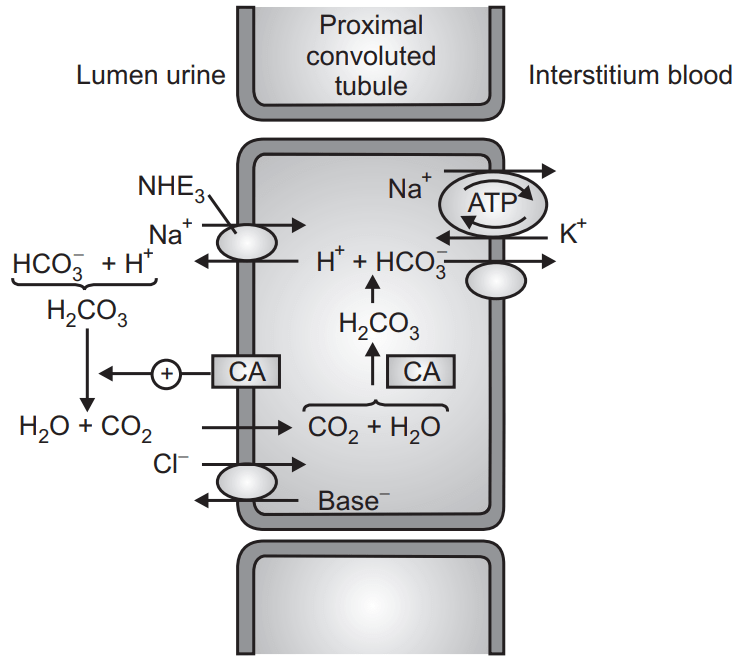
1. Carbonic Anhydrase Inhibitor:
Acetazolamide
Mechanism of Actions:
- Kidney: Self Limited Diuresis 2-3 days.
- Carbonic anhydrase catalyzes: CO2 + H2O → H2CO3
- H + ion produced by the breakdown of H2CO3 exchanged for Na+ and is also combined with HCO3− in the lumen of the PCT.
- Inhibition of Bicarbonate (HCO3−) reabsorption.
- Reduces Na+ – H+ -exchange NaHCO3 is excreted along with H2O.
Adverse Effects and Contraindications:
- Metabolic acidosis.
- Renal stones (Phosphate and Calcium stone).
- Renal potassium wasting; (NaHCO3−) enhances K+ secretion.
- Diuresis is self-limiting within 2-3 days.
- AE: Drowsiness, paresthesia, disorientation, renal stone (in case of urine alkalinization).
Contraindication:
- Liver cirrhosis (CA-I inhibits the conversion of NH3 to NH4) → NH3 increased → encephalopathy.
Indications of CA-I:
- Glaucoma (Eye: not self-limiting effect):
- Orally acetazolamide
- Topically dorzolamide, brinzolamide
- Prevent mountain sickness (high altitude) sickness inhibit sec of bicarbonate by the choroid plexus; Acidosis of the CSF results in hyperventilation.
- Urinary alkalinization: Preventing uric acid and cystine stones.
- Used for their diuretic effect only if edema is accompanied by significant metabolic alkalosis.
2. Thiazides:
- Hydrochlorothiazide (prototype), Chlorothiazide, Bendroflumethiazide, Chlorthalidone, Metolazone, Indapamide.
- All are sulfonamide derivatives, t1/2 − 6-12 hrs.
Mechanism of Actions:
- Thiazides are secreted by proximal tubules but works in DCT.
- Inhibit Na+ Cl symporter from the lumen to tubular cells → increase Na+ Cl– excretion (and water)
- Some thiazides have a weak CA-I effect.
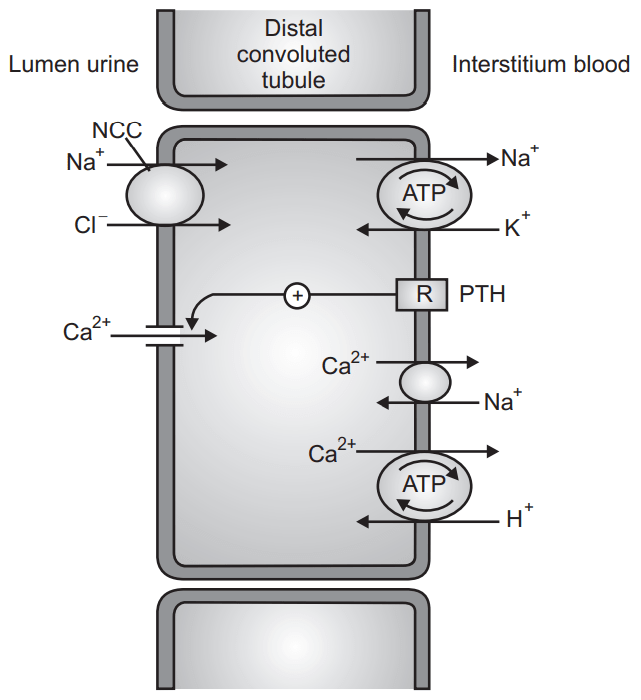
Effects on Electrolytes:
- Increases Na+ and Cl– excretion.
- Hypokalemic metabolic alkalosis; K+ excretion also increases associated with increased Na+ in distal tubules.
- Inhibits uric acid secretion → hyperuricemia and gout.
- Decreases Ca2+ excretion.
- Tends to increase plasma Ca++.
- Retards osteoporotic process.
- Increases Mg2+ excretion.
Adverse Effects:
- Hypo K+ → Increased risk of digitalis toxicity.
- Hypo Na+ , Hypo Mg++ .
- Hyperuricemia → caution in gout arthritis.
- Hyperglycemia and hypercholesterolemia are → not favorable for DM and dyslipidemia (although not contraindicated).
- Indapamide has fewer effects on lipid and uric acid.
- Hypercalcemia (long-term).
- Sexual dysfunction.
Interactions:
- Increases the risk of arrhythmia when combined.
- With digitalis, quinidine, and other antiarrhythmics.
- Reduces efficacy of anticoagulant and uricosuric.
- Reduces the efficacy of oral antidiabetics.
- NSAID reduce the efficacy of thiazide.
Indications of Thiazides:
- Hypertension (single drug or in combination).
- Chronic, mild-heart failure.
- Edema (loop diuretic is preferable).
- Nephrogenic Diabetes insipidus.
- Prevention of Ca++ excretion in osteoporosis and Calcium nephrolithiasis.
3. Loop Diuretics:
- Furosemide, torasemide, bumetanide: Are sulfonamide derivatives.
- Ethacrynic acid is a phenoxyacetic acid derivative.
- Site of action: thick ascending limb of Henle.
Mechanism:
- Loop diuretics should be excreted into the lumen.
- Inhibits Na+ , K+ , 2Cl– symporter → significantly increases the excretion of Na+ , K+ , Cl–
- Osmotic gradient for water reabsorption is also decreased → increasing water excretion.
- Ca2+ and Mg2+ are excreted as well.
Adverse effects:
- Hypovolemic metabolic alkalosis.
- Ototoxicity.
- Typical sulfonamide allergy.
Interactions:
- Concomitant use with aminoglycoside or cisplatin increases the risk of nephrotoxicity and ototoxicity.
- PGs are important in maintaining GF; NSAID reduces the effects of diuretics.
- Probenecid reduces the effects of diuretics by inhibiting its secretion into the lumen.
Indications:
- Congestive heart failure (1st line drug).
- Acute pulmonary edema.
- Edema due to renal failure, nephrotic syndrome, ascites.
- Hypercalcemia (that induced by malignancy).
- Severe hypertension.
- Forced diuresis during drug/chemical intoxication (a drug that is excreted through the kidney inactive form).
4. Potassium Sparing Diuretics:
(i) Na+ channel inhibitor (Amiloride, triamterene):
- Inhibit Na+ reabsorption → Na+ excretion.
- Reduced K+ secretion → K+ retention.
(ii) Aldosterone antagonist (Spironolactone, Eplerenone) Steroid Derivatives:
- Aldosterone induces the expression of Na/K ATPase and Na+ channel.
- Spironolactone and eplerenone block aldosterone receptor → reduces Na+ reabsorption and K+ secretion.
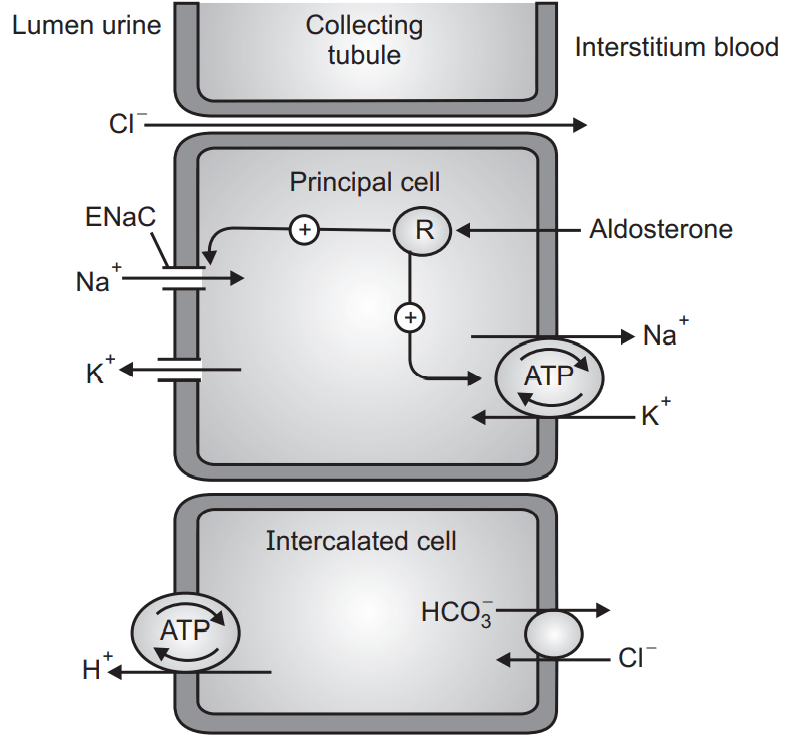
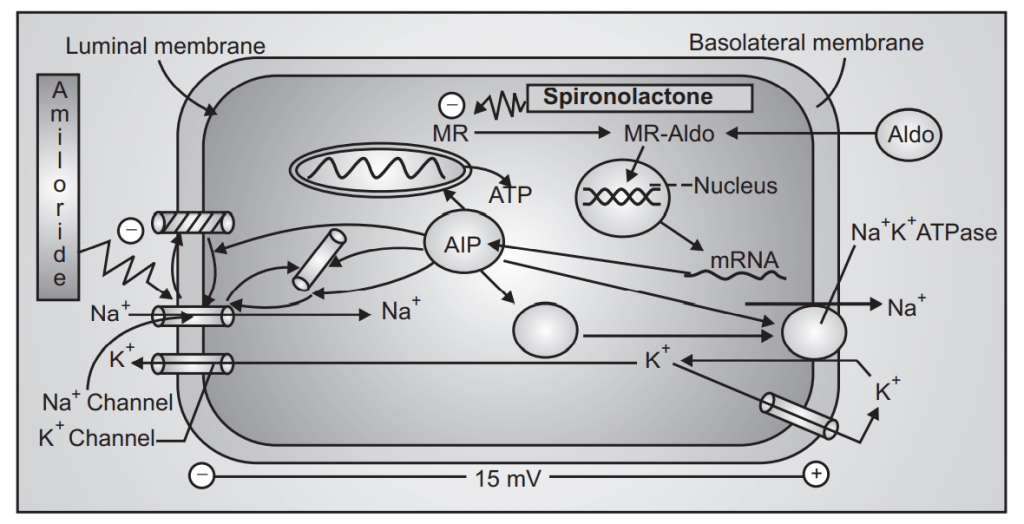
Fig.6: MoA of Potassium Sparing Diuretics
- Potassium sparing diuretic has a weak diuretic action.
- Usually used in combination with other diuretics:
- Potentiation of diuretic and antihypertensive effects.
- Prevents hypokalemia.
- Spironolactone is metabolized to its active metabolite, canrenone.
- Long-term use of spironolactone can prevent myocardial hypertrophy and myocardial fibrosis.
Adverse Effects:
- Hyperkalemia
- Antiandrogenic effect
- gynecomastia,
- decrease of libido, impotence,
- menstrual disturbance.
- Megaloblastic anemia: Triamterene (folate antagonist).
Indications:
- Antihypertension.
- In combination with other antihypertensives.
- To increase the effect and to prevent hypokalemia.
- Aldosteronism (that occurs in cirrhosis).
Contraindications/Precautions:
- Conditions that prone to hyperkalemia.
- Renal failure.
- Should never be combined with ACE-inhibition, ARB.
- NSAID, K+ supplementation.
5. Osmotic Diuretics (OD):
- Mannitol (prototype).
- Others rarely used: urea, glycerin, isosorbide.
- Properties of osmotic diuretics:
- Freely filtrated by the glomerulus.
- Negligible tubular reabsorption.
- Chemically inert.
- Usually non-metabolized.
Mechanism of Action:
- OD is filtrated and increases osmotic pressure in the tubular lumen.
- Hence, increases the excretion of water and electrolytes (Na+, K+, Ca++, Mg++, HCO3-, phosphate) ↑volume of urine and rate of urine flow through the tubule.
- Mannitol can also reduce brain volume and intracranial pressure by osmotically extracting water from the tissue into the blood.
- A similar effect occurs in the eye.
Adverse Effects:
- Removal of water from the I.C compartments → Initial increase of plasma volume → potentially dangerous in heart failure and pulmonary edema → Hypo → Na+ → headache, nausea, vomiting.
- Water excretion → Hypovolemia → Hypernatremia.
- Hypersensitivity reaction.
- Vein thrombosis, pain if extravasation (urea).
- Hyperglycemia, glycosuria (glycerin).
Pharmacokinetics:
- Mannitol and urea: Intravenous.
- Glycerin and isosorbide: Can be administered orally.
Metabolism:
- Glycerin 80% metabolized.
- Mannitol 20%.
- Urea, isosorbide: Not metabolized.
- Excretion: Renal.
Indications:
- Glaucoma (rare) ↓ IOP (Intra-Ocular Pressure).
- Brain edema, ↓brain volume, and pressure.
- Mannitol and urea are given before and after brain surgery.
- Disequilibrium syndrome after hemodialysis.
- Solute overload in severe hemolysis and rhabdomyolysis.
- Prophylaxis of ATN (acute tubular necrosis) due to contrast media, surgery, and trauma.
- NaCl 0.45% can also be used.
Make sure you also check our other amazing Article on : Plasma Volume Expanders