Excretion
Table of Contents
- Excretion is the process of elimination of substances from the body.
- Different waste products like urea, uric acid, creatinine, bilirubin, and ammonia are formed during various reactions taking place in cells.
- These waste products are break down products of protein metabolism, nucleic acid metabolism.
- These waste products should be eliminated from the body, accumulation of the same may lead to different disease conditions.
- The kidneys, large intestine, and skin are the important organs of excretion.
Waste products are excreted by different modes are as follows:
- Urine: Kidneys help to excrete urea, uric acid, creatinine, ammonia through urine. Excess amount of ions like Phosphates, Ca++, Na+, etc. is also excreted through urine. Many drugs, toxins, and even excess water are excreted through urine.
- Feces: Small amounts of water, inorganic salts, bacteria, products of bacterial decomposition, unabsorbed digested materials, and indigestible parts of food are excreted in feces. Most of the bilirubin in bile is metabolized in the small intestine by bacteria and eliminated in feces.
- Sweat: Very small amounts of salts, carbon dioxide, urea, and ammonia are excreted through sweat.
Human Excretory System
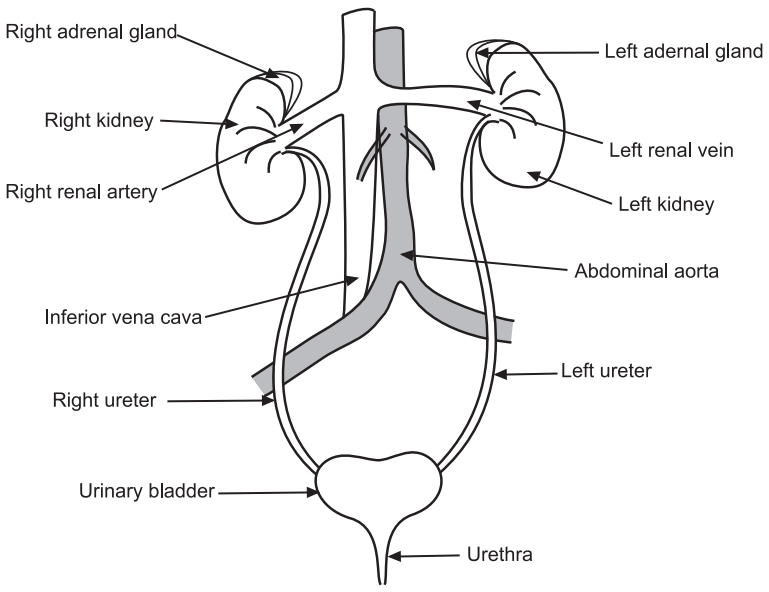
The human urinary system consists of two kidneys, two ureters, one urinary bladder, and one urethra. The kidneys are important organs of this system, the remaining parts are mainly connecting ducts or passageways and storage spaces.
Structure of Kidney
- A pair of the kidney is present just above the waist in the posterior wall of the abdomen. The kidneys are reddish, kidney-bean-shaped organs with a length of 10–12, a width of 5–7 cm, and a thickness of 3 cm.
- The renal hilum is the entry and exit site for structures servicing the kidneys: vessels, nerves, lymphatics, and ureters.
- Each kidney is surrounded by three layers of tissue namely, the renal capsule, Adipose capsule, and Renal fascia.
- A frontal section through the kidney reveals two distinct regions: The renal cortex and renal medulla.
- The outer, superficial area is called the renal cortex.
- The deep, inner region is called the renal medulla.
- The renal medulla consists of several cone-shaped regions called renal pyramids. The base of each pyramid faces the renal cortex. The apex of the renal pyramid is called the renal papilla. Renal papilla points toward the renal hilum.
- Renal columns are portions of the renal cortex that extend between renal pyramids.
- A renal lobe consists of a renal pyramid, its overlying area of the renal cortex, and one-half of each adjacent renal column.
- The functional portion of the kidney is called as parenchyma. Parenchyma is composed of the renal cortex and renal pyramids.
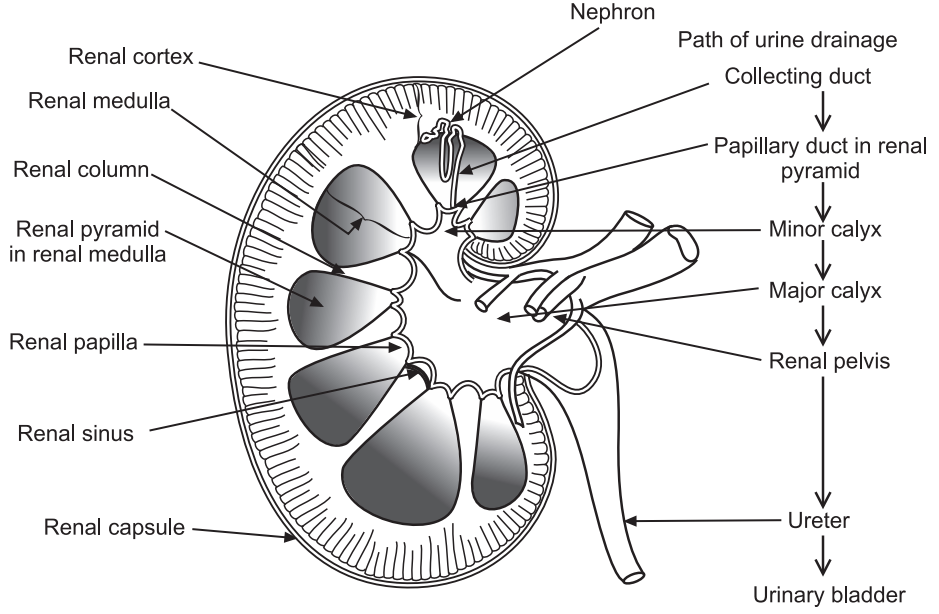
- Parenchyma consists of about 1 million microscopic structures called nephrons, which are the functional units of kidneys.
- Urine is formed by the nephrons.
- Urine formed is transferred to large papillary ducts, which extend through the renal papillae of the pyramids.
- The papillary ducts drain urine into cup-like structures minor calyx.
- Minor calyx transfers urine to the large major calyx.
- From the major calyces, urine is transferred to a single large cavity called the renal pelvis and then out through the ureter to the urinary bladder.
Structure of Nephron
Each nephron is made up of two parts:
- Renal corpuscle
- Renal tubule
1. Renal corpuscle: The Renal corpuscle is composed of two components:
- Glomerulus (capillary network).
- Glomerular (Bowman’s) capsule.
The Glomerular (Bowman’s) capsule is a double-walled epithelial cup that surrounds the glomerular capillaries.
Blood plasma is filtered in the glomerular capsule, and then the filtered fluid passes into the renal tubule, which has three main sections.
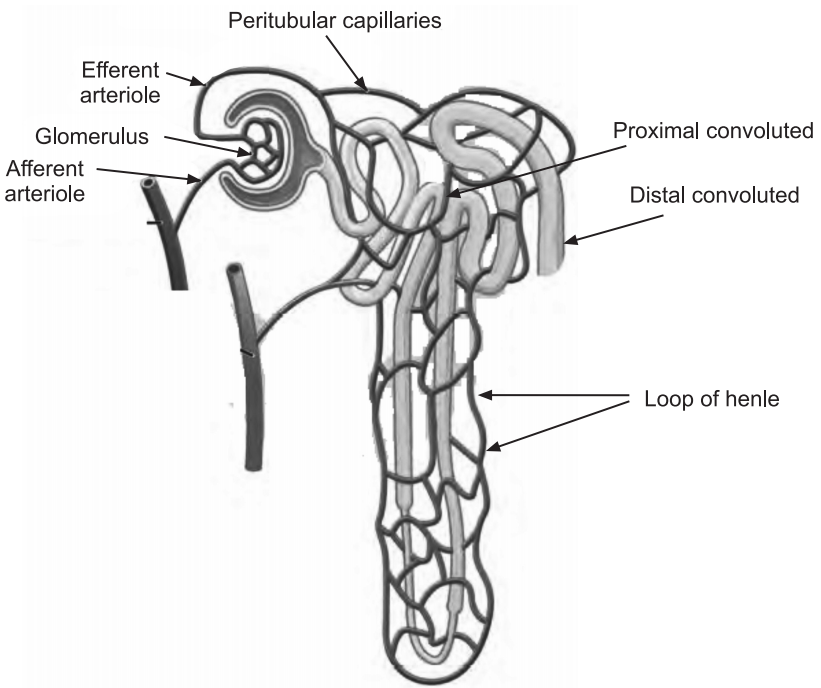
2. Renal tubule: The renal tubule is composed of three parts:
(i) Proximal convoluted tubule: This part is attached to the glomerular capsule.
(ii) Loop of Henle (nephron loop): This is the tightly coiled part of the renal tubule.
(iii) Distal convoluted tubule: This is the last part of the renal tubule.
- The renal corpuscle and both convoluted tubules lie within the renal cortex.
- The loop of Henle extends into the renal medulla, makes a hairpin turn, and then returns to the renal cortex.
- The distal convoluted tubules of several nephrons empty into a single collecting duct. Collecting ducts then unite and join into several hundred large papillary ducts, which drain into the minor calyces.
- The collecting ducts and papillary ducts extend from the renal cortex through the renal medulla to the renal pelvis.
Functions of Excretory System
- Kidneys play the following roles:
- Regulate blood volume and composition
- Help to regulate blood pressure
- Regulate pH
- Regulate glucose levels
- Produce two hormones (calcitriol and erythropoietin)
- Excrete wastes in urine
- A pair of ureters transport urine from the kidneys to the urinary bladder.
- Urinary bladder stores urine and expels it into the urethra.
- The urethra discharges urine out of the body.
Urine Formation
There are three steps in urine formation: glomerular filtration, tubular reabsorption, and tubular secretion.
1. Glomerular filtration: This is the first step of simple filtration. In this step, water and most solutes in blood plasma are filtered into the glomerular capsule and then transferred to the renal tubule.
2. Tubular reabsorption: In the second step, as filtered fluid flows along the renal tubule and through the collecting duct, tubule cells reabsorb about 99% of the filtered water and many useful solutes.
Here ‘reabsorption’ means the return of substances to the bloodstream. The term absorption, by contrast, means the entry of new substances into the body, as occurs in the gastrointestinal tract.
3. Tubular secretion: As fluid flows along the renal tubule and through the collecting duct, the tubule and duct cells secrete other materials, such as wastes, drugs, and excess ions, into the fluid. Tubular secretion takes away a substance from the blood.
Renin Angiotensin Aldosterone System
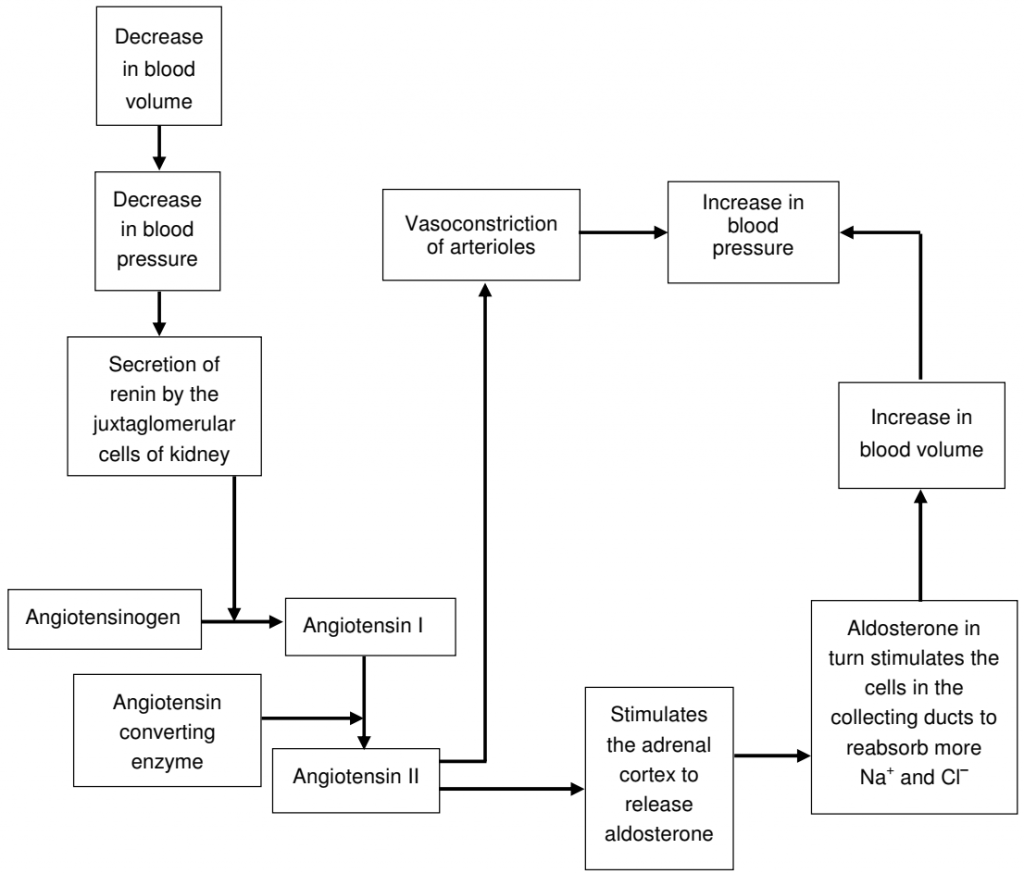
- Dehydration, Na deficiency, or hemorrhage leads to a decrease in blood volume.
- A decrease in blood volume decreases blood pressure. This decreased blood pressure leads to decreased stretching of the walls of the afferent arterioles. This leads to the secretion of the enzyme renin by the juxtaglomerular cells of the kidney into the blood.
- Renin converts a peptide, angiotensinogen (which is synthesized by the liver) to angiotensin I.
- Angiotensin-converting enzyme (ACE) converts angiotensin I to angiotensin II.
- Angiotensin II stimulates the adrenal cortex to release aldosterone, a hormone that in turn stimulates the cells in the collecting ducts to reabsorb more Na+ and Cl– and secrete more K+.
- Angiotensin II increases the reabsorption of Na+, Cl–, and water in the proximal convoluted tubule, which causes an increase in blood volume and blood pressure (BP).
- Angiotensin II causes vasoconstriction of arterioles which increases blood pressure and thus helps to raise blood pressure to normal.
Make sure you also check our other amazing article on : Digestion and Absorption
