Introduction of Gonorrhoea:
Table of Contents
Gonorrhoea is a sexually transmissible infection (STI) caused by bacteria known as Neisseria gonorrhoeae (gonococcus). It usually affects the genital area, although the throat or anus may also be affected. Gonorrhoea affects both men and women and is easily transmitted during vaginal intercourse. It can also be transmitted during anal or oral sex. Gonorrhoea is transmitted from any kind of sexual contact, including:
- Vaginal intercourse
- Anal intercourse
- Oral intercourse (both giving and receiving)
Pathophysiology of Gonorrhoea:
Gonococci are readily seen in smears (urethral, endocervical, or conjunctival exudates) and cultures, and appear as bean-shaped pairs, with the flat sides opposed. The organisms are cultured from tampons, urethral swabs, urine, specimens from the endocervix, vagina, anus, and pharynx.
Gonorrhoea begins as a surface infection of the mucous membranes, that is, a catarrh. The bacteria attach to and spread along with the cells of the surface mucous membranes, after which they invade superficially and provoke acute inflammation. The mucous membranes of the urethra, endocervix, and salpinx are characteristic sites.
The cell wall of Neisseria gonorrhoeae contains lipopolysaccharide, protein, and phospholipid. It lacks a true polysaccharide capsule, but projecting from the cell wall are hairlike extensions called pili. Within these pili is a protease that digests IgA on the surface of the mucus membrane, thus facilitating the attachment of gonococci to the columnar and transitional epithelium of the urogenital tract. “Smooth” strains with few pili are less virulent and less prone to cause urethritis or cervicitis. After an incubation period of 3 to 5 days, men usually have purulent urethral discharge and dysuria.
With prompt antibiotic treatment, the infection is arrested and gonococci are confined to the mucosa of the anterior urethra. However, if treatment is not instituted promptly, the organisms extend to the prostate, epididymis, accessory glands, where they cause urethral stricture, epididymitis, orchitis, and sometimes male infertility. Urethral stricture may be associated with fistulas between the urethra and perineum (“watering can” perineum). Male homosexuals develop pharyngitis and proctitis.
The first manifestation of infection in women is usually endocervicitis, with vaginal discharge or bleeding. There may be urethritis, manifested by dysuria rather than by urethral discharge. In some women (usually during the first menses after exposure), the infection extends to the fallopian tubes, where it produces acute and chronic salpingitis and pelvic inflammatory disease. The fallopian tubes swell with pus, causing acute abdominal pain. Infertility occurs when inflammatory adhesions close the tubes at both ends, blocking the ascent of sperm and the descent of ova. Infected fallopian tubes (‘pus tubes’) have the shape of a retort flask. From the fallopian tubes, the infection may spread to the peritoneum, healing as fine adhesions (“violin string” adhesions) between the capsule of the liver and the parietal peritoneum. The vaginal discharge may infect the anal crypts, leading to mucopurulent anal discharge, rectal pruritus, and tenesmus.
Chronic endometritis is a persistent complication of gonococcal infection and is usually a consequence of chronic gonococcal salpingitis. In such cases, the endometrium contains many lymphocytes and plasma cells.
Women (and to lesser extent men) may also develop bacteremia, producing disseminated gonococcal infection, which in turn leads to monoarthritis or polyarthritis. Neonatal infections from infected amniotic fluid or an infected birth canal result in symptoms within a few days after birth. These infections involve the conjunctiva and constitute a major cause of blindness. Other sites of neonatal infection are the pharynx, respiratory tract, vagina, anus, leptomeninges, joints, and blood.
Uncomplicated gonococcal infections of the urethra and endocervix are treated with penicillin and other antibiotics. Neisseria gonorrhoea is displaying increasing resistance to penicillin. Penicillinase-producing strains are especially common in Africa and Asia.
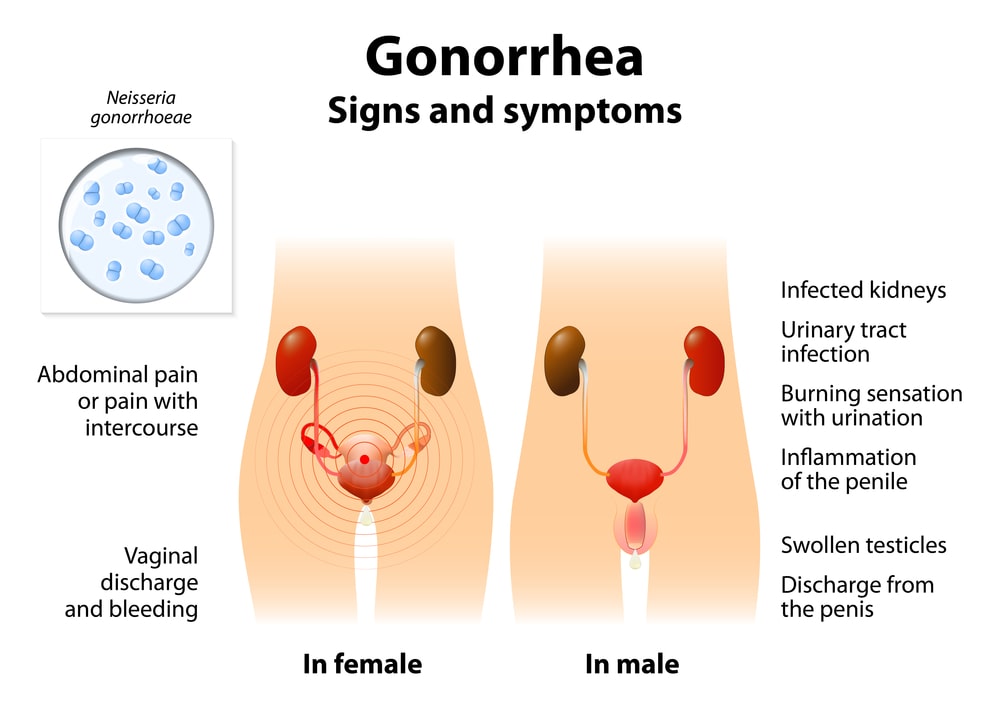
Signs And Symptoms:
Both men and women may have gonorrhoea without having any symptoms and so can be infected, or spread infection, without knowing anything is wrong. Some men never develop symptoms, but most do. Symptoms that may occur include:
- Throat and anal infections can occur following receptive oral and anal intercourse and infections at these sites are often without symptoms.
- Joint pain and infection (arthritis).
- Conjunctivitis (inflammation of the lining of the eyelids and eye) in both adults and children. Babies born to infected mothers can become infected as they pass through the infected cervix and may develop gonococcal conjunctivitis soon after birth.
- Having any sexually transmitted infection (STI) increases the risk of HIV infection if exposed to HIV while the other infection is present.
Men:
In addition to the above, gonorrhoea in men causes’ urethritis (infection of the urethra, the urinary canal leading from the bladder to exit at the tip of the penis) causing:
- A burning sensation in the penis when urinating.
- A white or yellow pus-like discharge from the penis (may be observed in underwear).
- Swelling and pain in the testicles, which can occur if the gonorrhoea infection goes untreated.
Women:
In addition to the above, gonorrhoea in women usually affects the cervix (opening of the uterus at the top of the vagina) causing:
- An unusual vaginal discharge.
- Discomfort on urination.
- Bleeding between periods, often after having sex.
- Pain while urinating or passing water.
The infection may spread from the cervix to the fallopian tubes, causing pelvic inflammatory disease (PID). Pelvic inflammatory disease due to gonorrhoea is often without symptoms, but there may be:
- Fever,
- Low abdominal pain,
- Pain on intercourse.
If untreated, the pelvic inflammatory disease may lead to scarring of the fallopian tubes and ectopic (tubal) pregnancy or infertility.
Risk Factors:
Risk factors for gonorrhea include the following:
- Sexual exposure to an infected partner without barrier protection (e.g., failure to use a condom or condom failure),
- Multiple sex partners,
- Male homosexuality,
- History of concurrent or past STDs,
- IV drug users,
- Use of crack cocaine,
- Early age of onset of sexual activity,
- Pelvic inflammatory disease (PID) – Use of an intrauterine device (IUD).
Diagnosis:
To determine whether the gonorrhoea bacterium is present in the body, analyze a sample of cells. Samples can be collected by:
- Urine test: This may help to identify bacteria in the urethra.
- A swab of the affected area: A swab of the throat, urethra, vagina, or rectum may collect bacteria that can be identified in a laboratory.
- Traditionally, gonorrhoea was diagnosed with gram stain and culture; PCR-based testing methods are common. All people testing positive for gonorrhoea should be tested for other sexually transmitted diseases such as chlamydia, syphilis, and human immunodeficiency virus.
Treatment:
Antibiotic resistance has developed to several agents, including macrolides, clindamycin, and rifampin. Ceftriaxone, a third-generation cephalosporin antibiotic, may be as effective as penicillin-based treatment.
CDC recommendation for uncomplicated gonorrhoea: Ceftriaxone 125 mg single IM dose or Ciprofloxacin 500 mg single oral dose plus doxycycline 100 mg twice daily for 7 days or Erythromycin 1 g single oral dose.
Prevention:
- Practice safer sex.
- No sex until antibiotic treatment is completed and the usual sexual partner has completed treatment.
- A follow-up test must be done to make sure that treatment has cleared the infection.
- All sexual partners need to be contacted, tested, and treated if indicated. Even if partners have no symptoms, they may be able to transmit the infection to other sexual partners.
- Testing to exclude other sexually transmitted infections is advisable.
Make sure you also check our other amazing Article on : Syphilis