Hematinics:
Table of Contents
- An agent that tends to stimulate blood cell formation or to increase the hemoglobin in the blood.
- Or used for the prevention and treatment of anemia.
Hemoglobin:
- Formed in the red bone marrow.
- It is a conjugated protein, consisting of an iron-containing pigment combined with histone (protein) is known as Globin.
- The iron-containing protein is a porphyrin consisting of 4 pyrrole rings.
- This porphyrin is designated as Heam.
- Folic acid and vitamin B12 are capable of increasing the rate of Heam synthesis in the red cells.
Anemia:
- A condition in which the blood is deficient in the RBC (erythrocytes), in hemoglobin.
- Or deficiency in quality or the quantity of blood.
- Erythrocytes are mainly responsible for delivering oxygen to the tissues, less RBC means less oxygen to tissues.
4 types:
- Microcytic anemia: Deficiency of iron (Fe).
- Macrocytic anemia: Deficiency of folic acid and B12.
- Hemolytic anemia: Abnormal breakdown of RBCs.
- Aplastic anemia: The body stops producing new blood cells.
Hematinics:
- IRON.
- FOLIC ACID (pteroylglutamic acid).
- VITAMIN B12 (cyanocobalamin).
IRON:
- The human body contains about 3.5 gm of iron of which about 2/3 is contained in the blood.
- 5 – 10% of ingested iron is absorbed.
- Once ingested the acid in the stomach:
1. Aids in ionization of iron
2. Splits chelated food iron from the chelator
3. Maintains iron insoluble form 4. Allows iron to remain in the absorbable form Fe3+.
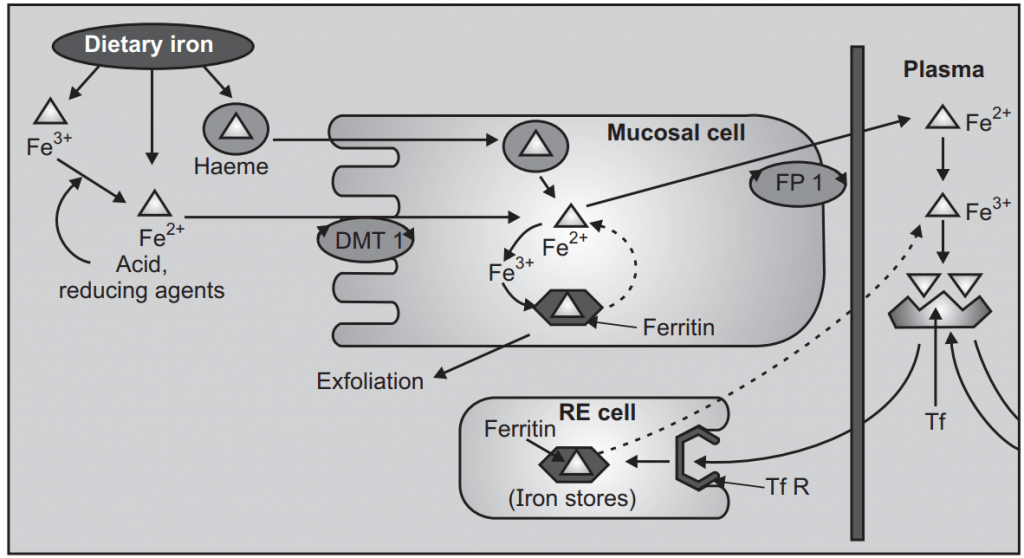
Mechanism of Iron Absorption:
- Iron absorption occurs all over the intestine.
- In the stomach, which contains HCL and reducing agent, convert the ferric to ferrous.
- Two separate iron transporters in the intestinal mucosal cells function to affect iron absorption.
- At the luminal membrane, the divalent metal transporter 1 (DMT) carries ferrous iron into the mucosal cell.
- The ferroportin is bound with ferrous iron and pass through mucosal cell directly into the bloodstream.
Transport, Utilization, Storage, and Excretion:
- As such, on entering plasma it is immediately converted to the ferric form and complexed with glycoprotein transferrin (Tf).
- Iron is transported into erythropoietic and other cells through the attachment of transferrin receptor (Tf Rs).
- The complex is engulfed by receptor-mediated endocytosis.
- Iron dissociates from the complex at the acidic pH of the intracellular vesicles.
- The released iron is utilized for hemoglobin synthesis or other purposes.
- Tf and Tf R are returned to the cell surface to carry fresh loads.
Storage:
- Reticuloendothelial cells
- Spleen
- Bone marrow
- Hepatocytes and myocytes.
Therapeutic uses of Iron:
- Iron Deficient Anemia
- Pregnancy
- Premature Babies
- Blood loss
- Hookworn infestation
- Malabsorption Syndrome
- GI Bleeding due to Ulcers, Aspirin, Excess consumption of coffee.
Iron Preparations:
Oral Iron:
- Ferrous Sulfate (Feosol) – 300 mg bid.
- Side Effects are extremely mild:
- Nausea, upper abdominal pain, constipation, or diarrhea.
- The cheapest form of Iron and one of the most widely used.
Parenteral:
- Iron Dextran (Imferon) – IM or IV
- Indicated for patients who cannot tolerate or absorb oral iron or where oral iron is insufficient to treat the condition ie. Malabsorption syndrome, prolonged salicylate therapy, dialysis patients.
FOLIC ACID
- A source of food – yeast, egg yolk, liver, and leafy vegetables.
- Folic Acid (F.A.) is absorbed in the small intestines.
- F.A. is converted to tetrahydrofolate by dihydrofolate reductase.
- Folic Acid deficiency (F.A. Deficiency) is also called Will’s Disease.
- Deficiency may produce megaloblastic anemia; neural tube defects in the fetus.
Therapeutic Uses of Folic Acid:
- Megaloblastic Anemia due to inadequate dietary intake of folic acid:
- Can be due to chronic alcoholism, pregnancy, infancy, impaired utilization: uremia, cancer, or hepatic disease.
2. To alleviate anemia that is associated with dihydrofolate reductase inhibitors:
- i.e. Methotrexate (Cancer chemotherapy), Pyrimethamine (Antimalarial)
- Administration of citrovorum factor (methylated folic acid) alleviates anemia.
3. Ingestion of drugs that interfere with intestinal absorption and storage of folic acid:
- Mechanism: Inhibition of the conjugases that break off folic acid from its food chelators.
- Example: Phenytoin, Progestin/estrogens (oral contraceptives)
4. Malabsorption: Sprue, Celiac disease, partial gastrectomy.
5. Rheumatoid arthritis: Increased folic acid demand or utilization.
Dose:
- Synthetic folic acid daily 10-30mg orally is given.
Toxicity:
- Non-toxic to man.
VITAMIN B12:
Source:
- In food, especially in the liver and kidneys. GI Microorganism synthesis, Vitamin Supplements (Cyanocobalamin).
- Necessary for normal DNA synthesis.
Absorption of B12:
1. Intrinsic Factor (low dose): A protein made by stomach parietal cells that bind to B12 and delivers it from the ileum via a calcium-mediated event.
2. Mass Action (High dose): 1000 mg/day, absorbed via passive diffusion.
Distribution of B12:
Vitamin B12 is distributed to various cells bound to a plasma glycoprotein, Transcobalamin II.
Storage of B12:
- Excess vitamin B12 (up to 300-500 microgram) is stored in the liver.
Therapeutic Uses of B12:
- Daily Requirements – 0.6 – 1.0mh/day; T1/2 ~ 1 year.
- Pernicious Anemia.
- Impaired GI absorption of B12.
- Gastrectomy.
- Corrosive Injury of GI mucosa.
- Fish tapeworm: worm siphons off B12.
- Placebo abuse with B12, especially in elderly patients.
- Malabsorption syndrome.
Make sure you also check our other amazing Article on : Therapy of Shock