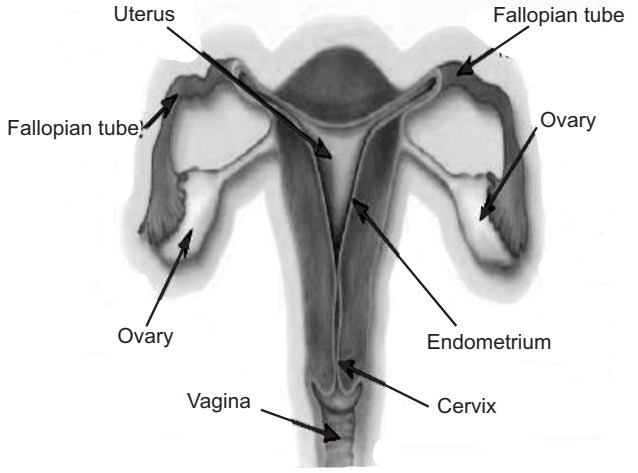
Anatomy of the Uterus: The uterus is a pear-shaped; thick-walled, muscular organ suspended in the anterior wall of the pelvic cavity.
- It measures normally about 3 inches long and 2 inches wide.
- Fallopian tubes enter its upper portion, one on each side, and the lower portion of the uterus projects into the vagina.
- The uterine cavity is normally triangular and flattened anterior-posteriorly. The wall of the uterus consists of three layers:
1. Endometrium: It is the inner coat of the uterine wall and is a mucous membrane that consists of epithelium lining and connective tissue. There are two types of arteries:
- Straight arteries: Supplies deeper layer.
- Coiled arteries: Supplies superficial layer.
2. Myometrium: It is a thick, muscular middle layer made up of bundles of interlaced, smooth muscle fibers embedded in connective tissue. It is subdivided into three ill-defined, intertwining muscular layers containing large blood vessels of uterine walls.
3. Peritoneum: It is the external surface of the uterus, which is attached to both sides of the pelvic cavity by blood ligaments through which the uterine arteries cross.
Intrauterine Devices (IUDs)
Table of Contents
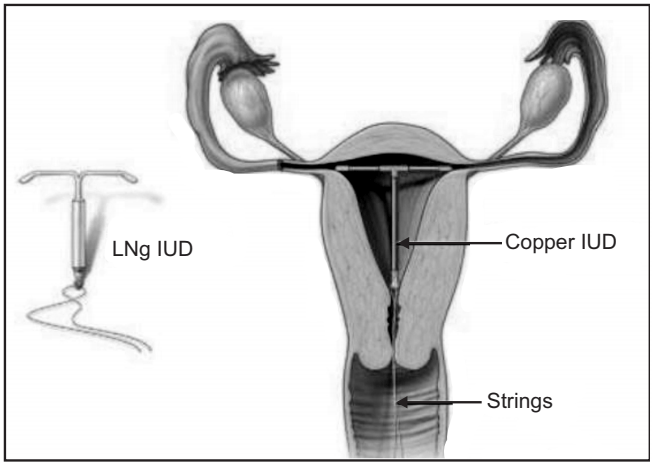
- It is a small object that is inserted through the cervix and placed in the uterus to prevent pregnancy.
- A small string hangs down from the IUD into the upper part of the vagina.
- IUDs show pharmacological efficacy for about 1-10 years. They work by changing the lining of the uterus and fallopian tubes affecting the movements of eggs and sperm so that fertilization does not occur.
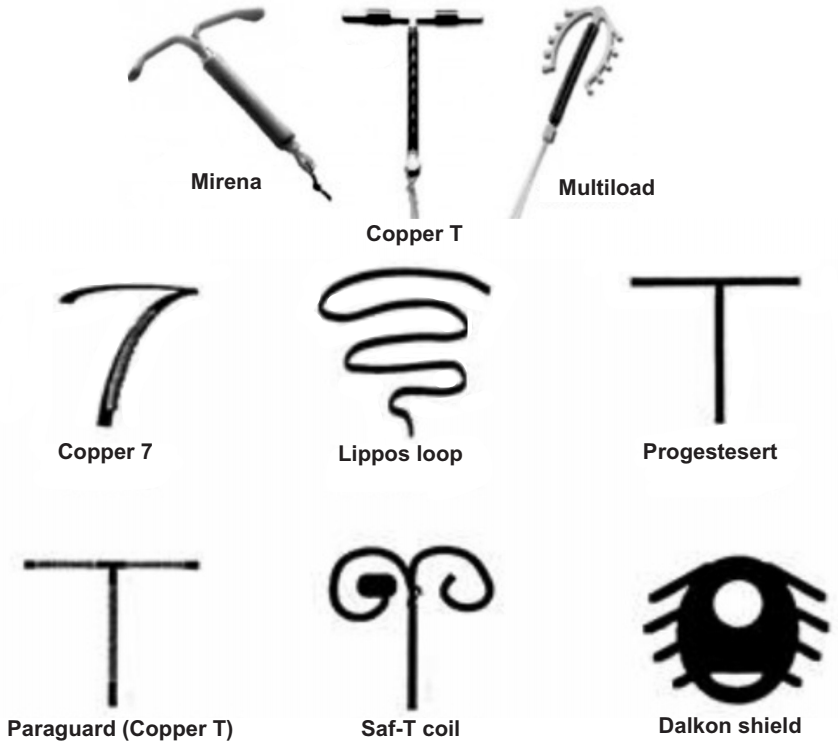
Development of IUDs
- These devices cause more endometrial compression and myometrial distention, leading to uterine cramps, bleeding, and expulsion of IUDs.
- Researchers developed IUDs in the past 30 years to add antifertility agents to more tolerated, smaller devices, such as T-shaped devices, to enhance effectiveness; or antifibrinolytic agents, such as e-aminocaproic acid and tranexamic acid to larger IUDs to minimize the bleeding and pain.
- Tatum developed a T-shaped device that would work better with the shape of the uterus, which forms a T when contracted. This reduced side effects significantly.
- Zipper 1968 added contraceptive metals (Cu) and Doyle and Clewe developed Progestin releasing IUD.
- This development initiated a new era of R and D for long-term IU contraception, leading to the generation of recent IUDs-medicated IUDs.
- Copper-bearing IUDs such as Cu-7 and Progesterone releasing IUDs such as Progestasert (approved by FDA in 1976) thus evolved.
Types of IUDs
- Non-medicated IUDs
- Medicated IUDs
1. Non-medicated IUDs: These exert their contraceptive action by producing a sterile inflammatory response in the Endometrium by its mechanical interaction. These do not contain any therapeutic effect. E.g. Ring-Shaped IUDs of Stainless Steel, Plastic IUDs, Lippes Loop, Dalkon Shield, Saf-T-Coil.
2. Medicated IUDs: These are capable of delivering pharmacologically active antifertility agents. E.g. Copper bearing IUDs, Progesterone releasing IUD.
There are two types of medicated IUDs:
- Copper bearing IUDs.
- Hormone releasing IUDs: There are two types:
- Progesterone releasing IUD – Progestasert.
- Levonorgesterone IUD – Levonorgestrel releasing device – [MIRENA].
Advantages of IUDs
The IUD is one of the most popular contraceptive methods, especially for long-term reversible contraception, as it can be easily fitted and removed.
- It is highly effective, with a 98-99% success rate over five years of IUD use.
- It can be used by almost any woman including nulliparous.
- Its action lasts for ten years if it is not removed in between.
- The onset of action is immediate.
- It is suitable for lactating women.
- Fertility returns promptly on discontinuation.
- It can be used by women who are on any type of medication.
- It is not associated with cancer of any organ, unlike hormonal contraception.
- It is cost-effective.
Disadvantages of IUDs
- Menorrhagia is a frequent complaint, as are dysmenorrhoea and polymenorrhoea. These are the major reasons for IUD discontinuation.
- It does not offer any protection against sexually transmitted infections (STIs).
- There is a slight risk (1%) of acquiring a uterine infection during IUD insertion within 20 days of the procedure. This is increased if the woman is prone to STIs. Women should be tested for gonorrhea or chlamydia before insertion, and for any other organism if they so request. Fortunately, pelvic infections with the IUD in utero can be treated adequately without removing the device.
- Expulsion of the IUD may occur especially following or during the periods in the first three months.
- Uterine perforation may occur in 0.1% of women during insertion. This may manifest as lower abdominal pain. Perforation will require surgical removal.
- There is a higher risk of ectopic pregnancy if conception occurs with an IUD in situ, though pregnancies are very rare with this method.
- Nausea, Vomiting, Headache, and Weight gain are some of the side effects.
Applications
- It is used as a contraceptive to prevent pregnancy.
- It can be suitable for use in Hormone Replacement Therapy.
- It can be safely used in women with heavy bleeding to prevent/control the same.
- In the treatment of fibroids.
Make sure you also check our other amazing Article on : Monoclonal Antibodies
