INTRODUCTION of NSAIDs
Table of Contents
- NSAIDs (Non-steroidal anti-inflammatory drugs) are the groups of drugs that reduce pain, decrease fever, and, in higher doses, decrease inflammation, they are less potent than a narcotic analgesic.
- These are also called non-narcotic analgesics.
- They reduce dull aching pain but not useful in visceral pain.
- Useful in the treatment of postoperative, dental, menstrual pain, Muscle pain, Joint pain, headaches, and migraine.
- They possess non-narcotic analgesic, antipyretics, and anti-inflammatory action.
Non-narcotic analgesic: Reduced pain without CNS depression.
Antipyretics: Which reduces elevated body temperature.
Anti inflammatory: Useful to produced symptomatic relief from pain.
CLASSIFICATION of NSAIDs
(A) Nonselective COX Inhibitors (Traditional NSAIDs)
1. Salicylates: Aspirin, Methyl Salicylate, Sodium salicylate.
2. Propionic acid derivatives: Ibuprofen, Naproxen, Ketoprofen, Flurbiprofen.
3. Anthranilic acid derivative: Mefenamic acid, Enfenamic acid, Flufenamic acid.
4. Aryl-acetic acid derivatives: Diclofenac, Aceclofenac.
5. Oxicam derivatives: Piroxicam, Tenoxicam.
6. Pyrrolo-pyrrole derivative: Ketorolac.
7. Indole derivative: Indomethacin, Sulindac.
8. Pyrazolone derivative: Phenylbutazone, Oxyphenbutazon.
(B) Preferential COX-2 Inhibitors:
Nimesulide, Meloxicam, Nabumetone.
(C) Selective COX-2 Inhibitors:
Celecoxib, Etoricoxib, Parecoxib.
(D) Analgesic-antipyretics with Poor Anti-inflammatory Action:
1. Para aminophenol derivatives: Paracetamol, Phenacitn.
2. Pyrazolone derivative: Metamizol, Propiphenazone.
3. Benzoxazocine derivative: Nefopam.
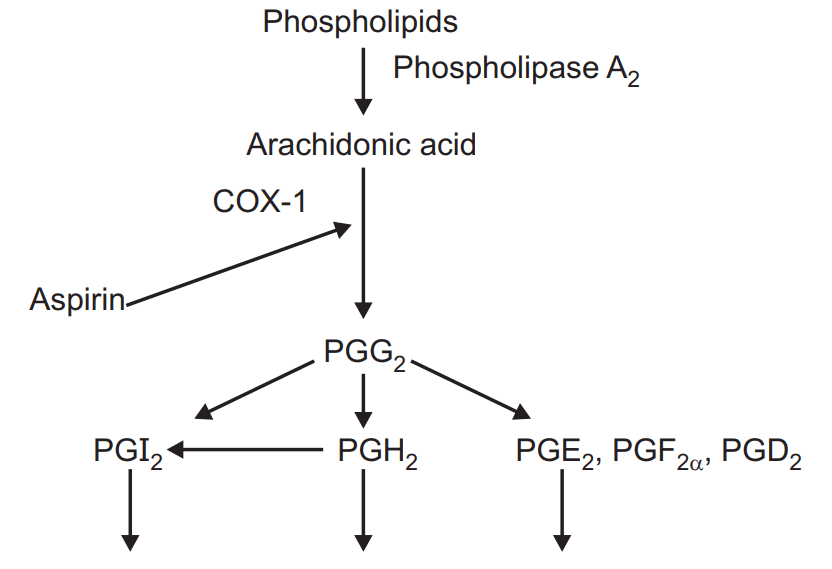
MECHANISM OF ACTION of NSAIDs
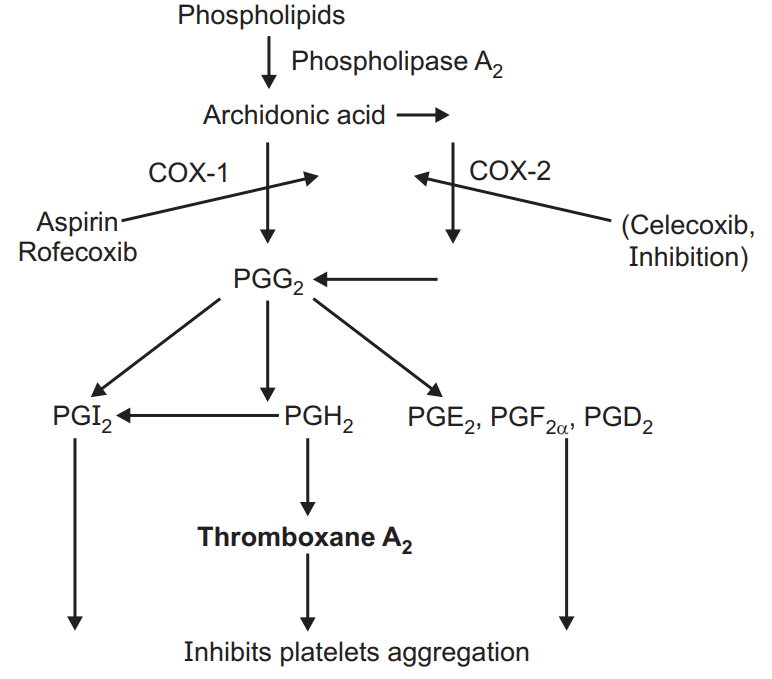
- Inhibits Platelets aggregation
- Inhibits pain sensation – Analgesic action.
- Reset hypothalamus at a lower temperature – Antipyretic action.
- Reduced capillary permeability, Decreased tissue edema – Anti-inflammatory action.
COX inhibitors cause inhibition of COX enzyme and inhibit the conversion of Arachidonic acid into PGG2 later PGG2 to PGH 2, PGI 2, PGE2, PGF2α, PGD2, and Thromboxane A2.
So result: Inhibits pain sensation – Analgesic action, Reset hypothalamus at a lower temperature – Antipyretic action, reduced capillary permeability, decreased tissue edema – Anti-inflammatory action and inhibits pain sensation – Analgesic action.
PHARMACOLOGICAL ACTIONS of NSAIDs
Analgesic effect:
The analgesic effect by:
- Peripheral inhibition of prostaglandin production.
- May also be due to the inhibition of pain stimuli at a subcortical site.
- It also inhibits the pain sensitizing mechanism induced by TNFα and Bradykinin.
- Prevent the potentiating action of prostaglandins on endogenous mediators of peripheral nerve stimulation.
- Aspirin is a weaker analgesic than morphine-type drugs.
- Effectively relieves inflammation, tissue injury, connective tissue, and integumental pain, but is relatively ineffective in severe visceral and ischaemic pain.
- No sedation, subjective effects, tolerance, or physical dependence.
Antipyretic effect:
- Inhibition of the production of prostaglandins induced by interleukin-1 (IL-1) and interleukin-6 (IL-6) in the hypothalamus.
- “Resetting” of the thermoregulatory system, leading to vasodilatation and increased heat loss.
Anti-inflammatory effect:
- Due to the inhibition of the enzymes that produce prostaglandin (cyclooxygenase, or COX), which converts arachidonic acid to prostaglandins, and TxA2 and prostacyclin.
- Inhibits accumulation of fluids.
- Reduced capillary permeability.
- Reduced exudation of fluid.
- Reduced tissue swelling.
- Result anti-inflammatory effect.
Metabolic and Endocrine effects:
- Significant only at anti-inflammatory doses (High dose).
- Cellular metabolism is increased, especially in skeletal muscles, due to the uncoupling of oxidative phosphorylation.
- Increased utilization of glucose blood sugar may decrease and liver glycogen is depleted.
- Chronic use of large doses causes negative N2 balance by increased conversion of protein to carbohydrate.
- Plasma-free fatty acid and cholesterol levels are reduced.
- It stimulates the adrenal medulla and increases adrenaline secretion which intern produced hypoglycemia.
Respiratory System:
- Effects are dose-dependent.
- It increased the consumption of oxygen by skeletal muscles and increased the production of carbon dioxide.
- It stimulates medullar respiratory centers so result increased rate of respiration.
- At anti-inflammatory doses, respiration is stimulated by peripheral (increased CO2 production) and central (increased sensitivity of respiratory center to CO2) actions.
- Hyperventilation is prominent in salicylate poisoning.
- Further rise in salicylate level causes respiratory depression; death is due to respiratory failure.
Acid-base and Electrolyte Balance:
- Anti-inflammatory doses produce significant changes in the acid-base and electrolyte composition of body fluids.
- Initially, respiratory stimulation predominates.
- Still higher doses cause respiratory depression with CO2 retention, leading to respiratory acidosis.
CVS:
- Aspirin has no direct effect in therapeutic doses.
- Larger doses increase cardiac output to meet increased peripheral O2 demand and cause direct vasodilatation.
- Toxic doses depress vasomotor center: BP may fall.
- Because of increased cardiac work as well as Na+ and water retention, CHF may be precipitated.
- Decreased prothrombin levels and inhibits platelet aggregation.
Blood:
- Aspirin irreversibly inhibits TxA2 synthesis by platelets, bleeding time is prolonged to twice.
- Long-term intake of large dose decreases synthesis of clotting factors in liver and predisposes to bleeding; can be prevented by prophylactic Vit. K therapy.
GIT:
- Aspirin and released salicylic acid irritate gastric mucosa, cause epigastric distress, nausea, and vomiting.
- It also stimulates CTZ.
- Prolonged use may lead to ulcer formation as it inhibits PGE2, PGF2α synthesis, which intern inhibits gastric mucosa production.
Kidney:
- It inhibits PGE2, PGF2α results in decreased glomerular filtration and decreased urine outputs.
- It also increases Na+ and Water retention, which leads to increased BP and edema formation.
Local Action:
- It produced fungistatic, keratolytic and antiseptic action.
- It caused irritation of GIT which leads to nausea and vomiting.
Pharmacokinetics:
- Absorbed from the stomach and small intestines.
- Poor water solubility is the limiting factor in absorption: micro fining the drug particles and inclusion of an alkali enhances absorption.
- 50-60% binds to plasma protein.
- Rapidly deacetylated in the gut wall, liver, plasma, and other tissues to release salicylic acid which is the major circulating and active form.
- Slowly enters the brain but freely crosses the placenta.
- The metabolites are excreted by glomerular filtration as well as tubular secretion.
Therapeutic Uses:
- Analgesic.
- Antipyretic.
- Acute rheumatic fever.
- Rheumatoid arthritis.
- As antiplatelet agents.
- Local application for Fungistatics, Antiseptics, and Keratolytics.
Adverse Effects:
- GIT – Nausea, vomiting, Diarrhoea, Ulceration, perforation, and hemorrhage.
- Intolerance – Skin rashes, urticaria, pruritis, bronchial asthma, anaphylactic shock.
- Bone marrow depression – Agranulocytosis, Thrombocytopenia, Aplastic anemia.
Precautions to be taken while using Aspirin:
- It should not be taken on an empty stomach.
- Patients suffering from ulceration.
- During delivery as it increases bleeding time.
- Allergic or sensitive to salicylates.
Salicylism:
- Headache, Tinnitus, Giddiness, Difficulty in hearing, Mental confusion, vomiting, diarrhea, respiratory alkalosis.
Acute poisoning:
- Hyperglycemia, acidosis, dehydration, GIT irritation, hemorrhage, restlessness, excitement, delirium, tremors, euphoria, convulsion, hallucination.
Treatment:
- Gastric lavage.
- Correction of dehydration, acid-base balance.
- Administration of alkalies and fluids (0.9% saline with 2% NaHCO3) prevents metabolic acidosis and increased excretion of salicylates.
PARACETAMOL
- Most commonly used as antipyretics and analgesics effects.
- Analgesic – one of the most commonly used non-narcotic antipyretic agents.
- Weak anti-inflammatory activity.
- Effects of does not share the gastric or platelet side the other NSAIDs.
- Inhibits Prostaglandins synthesis.
- Inhibition of the production of prostaglandins induced by interleukin-1 (IL-1) and interleukin-6 (IL-6) in the hypothalamus.
- Reset hypothalamus at a lower temperature – Antipyretic action.
Pharmacokinetics:
- Well absorbed when given orally, with min. 30-60 in reaching concentrations plasma peak.
- The plasma half-life of therapeutic doses is 2-4 h.
- Paracetamol is metabolized to N-Acetyl P-benzoquinone imine and inactivated in the liver, being conjugated to give glucuronide.
- Excreted in urine.
Therapeutic Uses:
- Analgesics
- Anti-pyretic
Adverse Effects:
- With therapeutic doses, side effects are few and uncommon.
- Allergic skin reactions.
- Regular intake of large doses over a long period causes kidney damage.
- Toxic doses cause potentially fatal hepatotoxicity.
SELECTIVE COX-2 INHIBITORS
Celecoxib and Etoricoxib
- Symptomatic relief in the treatment of osteoarthritis and rheumatoid arthritis.
- Extensively metabolized in the liver.
- High plasma protein binding.
- Dizziness, skin. Common adverse effects are headaches, rashes, and peripheral edema caused by fluid retention.
Parecoxib:
- Prodrug of valdecoxib.
- Short-term treatment of postoperative pain.
- Plasma protein binding is high.
- The drug should also be given with caution to patients with impaired renal function, and renal failure has been reported.
- Postoperative anemia may also occur.
Make sure you also check our other amazing Article on : Autacoids and Related Drugs