Patient Medication History Interview: Patient medication history interview is a practice associated with the collection and recording of information by reviewing/interviewing of patient-related to his/her past and present medications used. Clinical pharmacists are mainly responsible/dealing with such type of activity. Clinical pharmacist collects detailed, accurate, and complete information on all prescribed and non-prescribed medications that patients have taken previously or currently under use.
Patient medication history provides valuable information on the patient’s allergic tendency, patient compliance, and self-medications. Such type of practice helps the pharmacist to establish with a patient, commence patient counseling, and design a pharmaceutical care plan.
Goals And Need of Patient Medication History Interview
Table of Contents
The goal of a medication history interview is to acquire information on aspects of drug use by patients. So, such information may help pharmacists for improvement in the overall care of a patient. The collected information can be helpful to achieve the following goals:
- Helps to investigate the medication discrepancies by comparing the medication profile with the medication administration record.
- Other staff verify the collected history of a patient and can provide additional information wherever require appropriately.
- Helps to document the allergies and drug-related adverse reactions.
- Helps to evaluate the rationale for prescribing drugs.
- Helps to assess indications of drug abuse.
- Helps to check the drug interactions.
- Helps to access drug administration techniques.
- Helps to examine the requirement of assistance in medication.
Importance of Accurate Medication History:
- Helps in the prevention of prescription errors and subsequent risks to the patients.
- Helpful in a finding of drug-related pathology and any clinical signs due to results of drug therapy.
- Considering all accurate medication history information helps to establish a better care plan for the patients.
Stages of Patient Medication History
There are three stages involved while practicing for patient medication history. The objective and procedure at each stage are discussed below:
Stage 1: Before taking medication history.
Objective: To create good relationships and build confidence in patients.
Method: Following are different steps in this procedure:
- Confirmation of patient identity.
- Self-Introduction.
- Reason of interrogation and total time required for interrogation.
- Initiate in taking of medication history of a patient.
Stage 2: During taking of history.
Objective: To collect accurate information on the medication history.
Method: Following is the step followed in this stage.
- Ask the question according to the format given for the collection of medication information.
Stage 3: After taking history.
Objective: Documentation and analysis of information.
Method: Following are steps follow in this stage:
- After completion of the interview, a pharmacist must express appreciation for providing this information.
- Review and analyzes the past medical record.
- Documentation of important medication history data of a patient.
Type of Information Need to Be Recorded
The following information is commonly recorded while interviewing the patient for the collection of medication information:
- Recently prescribed medicines.
- Use of OTC medication.
- Any vaccinations in past or recently.
- Any social habit (e.g. Alcohol, smoking).
- Any Use of traditional medicines.
- Any reactions and allergies occur due to the use of medicine.
- Medicines were found to be ineffective.
- Compliance with past treatment.
- Use of any techniques/assistances in drug administration or medication adherence.
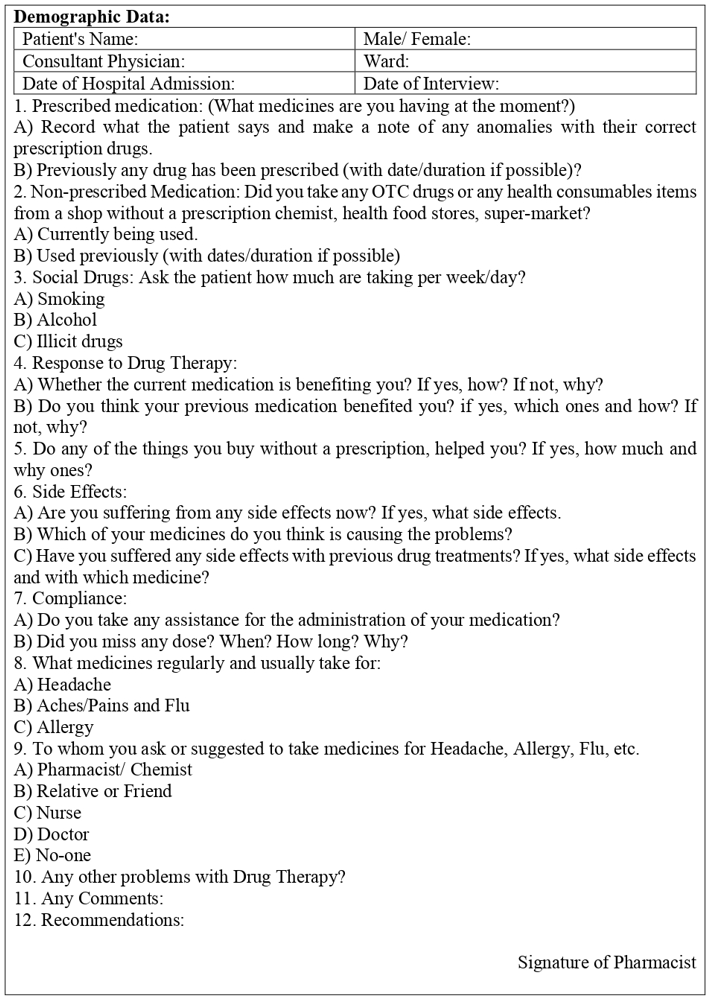
A pattern of Questions To Be Asked By Pharmacist In Interview
Following are some questions patterns that may be asked by pharmacists while a collection of information on the medication history. Format for the Medication History Interview form is given at the end of this chapter.
Which medications are you have taken or are currently taking:
- The name of the medication used.
- Type of dosage form.
- Dose of medication.
- How are they taking it (by which route)?
- How many times take in a day?
- For what reason you are taking medications?
- Any allergic reactions were seen with medications and what was the reaction?
- Are you taking any medicine on a regular/needed basis? If yes, for what reason?
- Any counter medications are you taking on a regular or as-needed basis? If yes, for what reason?
- Any traditional medicines are you taking on a regular or as-needed basis? If yes, for what reason?
- Any vitamins or other supplements are you taking? If yes, for what reason?
- Have you taken any new medicine?
- Are there any changes in dose or stop of medication by a doctor recently?
- Recently did you minimize the doses or stop any of your medications?
- Are any of the medications producing any kind of side effects?
- Did you stop or change any medications due to unwanted side effects/feel worse?
- Did you stop taking your medicine sometimes whenever you feel better?
Medication History Interview Form
Make sure you also check our other amazing Article on : Therapeutic Drug Monitoring
