Introduction of Peptic ulcers:
Table of Contents
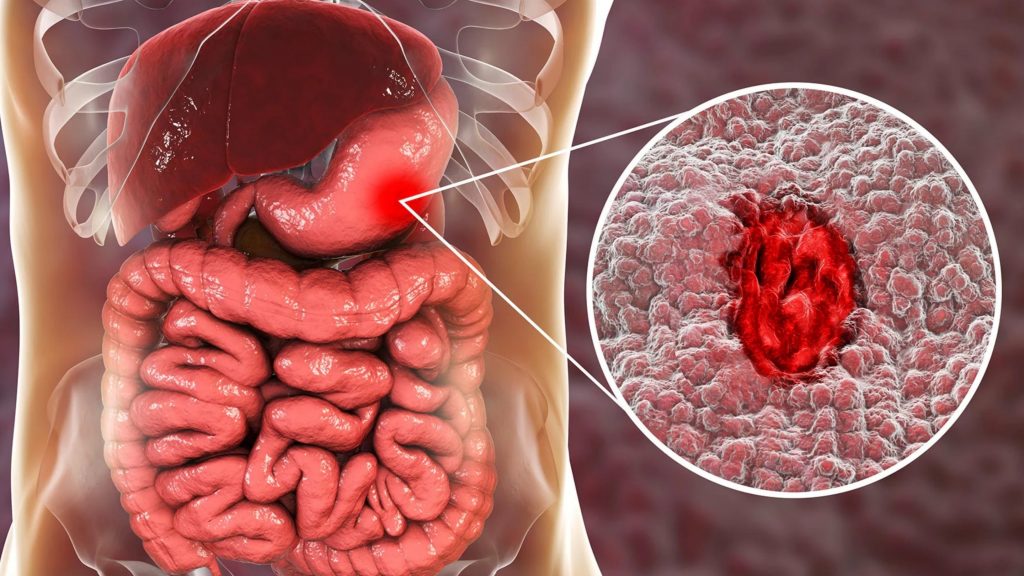
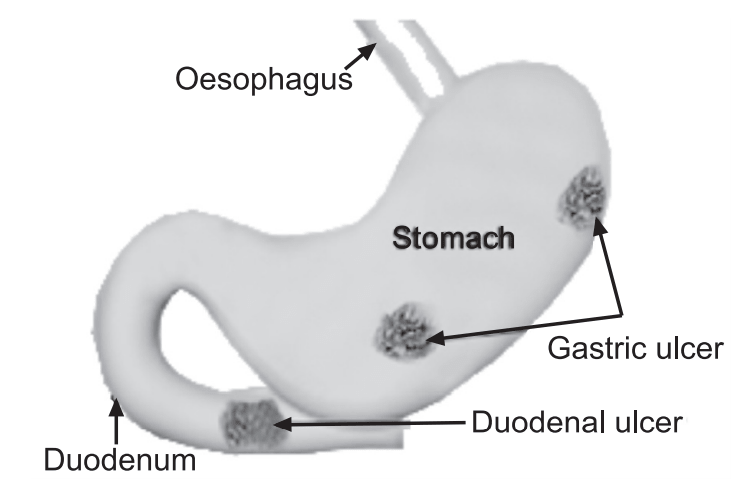
Peptic ulcers are open sores that develop in the inside lining of the esophagus, stomach, and upper portion of the small intestine (duodenum) as a result of erosion from stomach acids. A peptic ulcer of the stomach is called a gastric ulcer of the duodenum, a duodenal ulcer; and of the esophagus, an esophageal ulcer. Peptic ulcers occur when the lining of these organs is corroded by the acidic digestive (peptic) juices which are secreted by the cells of the stomach. A peptic ulcer differs from erosion because it extends deeper into the lining of the esophagus, stomach, or duodenum and excites more of an inflammatory reaction from the tissues that are eroded. It is an ulcer of the gastrointestinal tract in an area exposed to the acid pepsin mixture (APM). The mucosa of the gastrointestinal tract (GIT) in this area is digested by pepsin (peptic digestion). It is most often caused by Helicobacter pylori infection.
The vast majority of peptic ulcer occurs in
1. Stomach (Gastric ulcer).
2. First part of duodenum (Duodenal ulcer).
3. Lower end of the esophagus (as a result of reflux from the stomach into the esophagus).
The ratio of incidence in duodenal ulcer and peptic ulcer is 4:1.
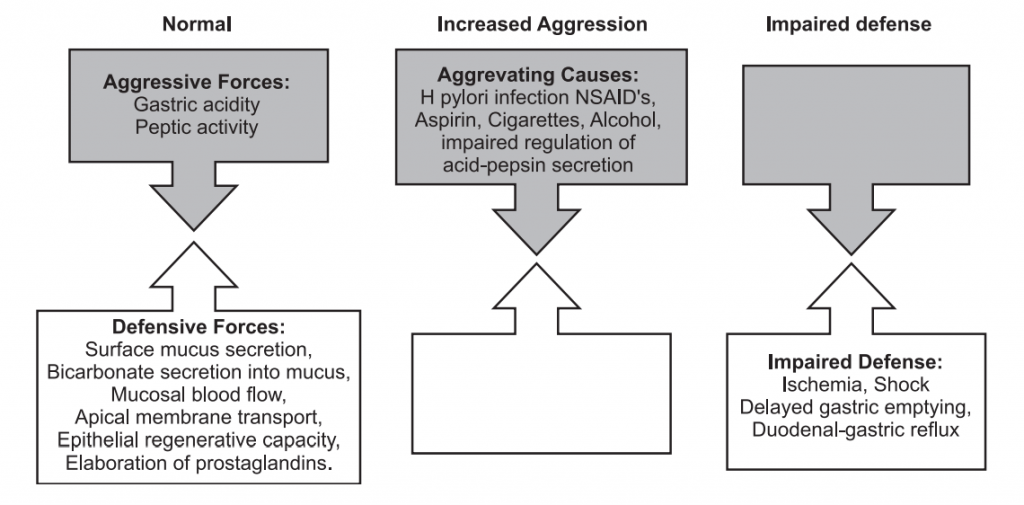
Components of Gastric Defense Mechanism:
A. Gastric mucus and bicarbonate secretion by gastric mucosal cells: Gastric mucus forms a layer over the epithelium of mucosa. Mucosal cells of the pyloric region secrete bicarbonate ions which remain in between the epithelial cells and the mucus and pH at this region is 6 or 7. In the luminal surface of the mucus, the pH is low i.e. 2-3, therefore the peptic activity is high, digestion is possible. Near the epithelium, deep to the mucus layer, the pH is high therefore pepsin loses its activity.
The mechanical barrier offered by mucus present over the surface of gastric epithelium is an important component of defense. The mucus is thick and sticky, APM fails to penetrate it, and no digestion of epithelial cells. Pepsin is a big molecule and it requires a good deal of space through which it transverse. Aspirin and non-steroidal anti-inflammatory agent can depolymerizes and causes loss of their stickiness and increases permeability to pepsin.
B. Presence of tight junction between epithelial cells of stomach and duodenum: Presence of tight junction between epithelial cells of stomach and duodenum restrict the entry of material but high acidity of aspirin is better absorbed in the stomach and damage the tight junction leads to peptic ulceration.
Components of Aggressive Mechanism:
1. Helicobacter pylori (H. Pylori): It is a gram –ve bacteria found in gastric and duodenal mucosa of most people, particularly the elderly. They, while in the mucosa, split urea into ammonia and thus elevate the local pH and damage the local region of the mucosa by high alkalinity. In this way, they strongly help the peptic ulcer development (PUD).
2. Acid: Hydrochloric acid (HCl) is secreted by the parietal cells of the gastric glands. Excess acid production from gastrinomas (it is a tumor in the pancreas or duodenum that secretes an excess of gastrin leading to ulceration), tumors of parietal cells of the stomach increases acid output.
3. Non-steroidal anti-inflammatory drugs (NSAID): Non-steroidal anti-inflammatory drugs, such as aspirin, naproxen, ibuprofen, and many pain medications can irritate or inflame the lining of the stomach and small intestine. Even safety coated aspirin and aspirin in powdered form can frequently cause ulcers.
4. Stress: Emotional stress is no longer thought to be a cause of ulcers, however, people with ulcers often report that emotional stress increases ulcer pain.
Physical stress may increase the risk of developing ulcers, particularly in the stomach. For example, people with injuries, such as severe burns, and people undergoing major surgery often require treatment to prevent ulcers and ulcer-related complications, such as bleeding.
5. Genetics: A significant number of individuals with peptic ulcers have close relatives with the same problem, suggesting that genetic factors may also be involved. The genetic disorder Zollinger-Ellison syndrome (ZES) is responsible for some ulcers. Zollinger-Ellison syndrome is a rare disorder in which tumors secrete large amounts of the hormone gastrin. This hormone causes the stomach to produce excess acid which attacks the lining of the stomach and causes ulcers.
6. Smoking: People who regularly smoke tobacco are more likely to develop peptic ulcers compared to non-smokers.
7. Alcohol consumption: Regular heavy drinkers of alcohol have a higher risk of developing peptic ulcers.
In a normal person, the defense mechanism is adequate, no ulcer develops. Where the defense mechanism is weakened, or, is the aggressive mechanism, i.e. APM strengthened, peptic ulcer develops.
Stimulants/Inhibitors of HCl Secretion: Parietal cells are supplied by vagal fibers. Stimulation of the vagus causes HCl secretion from parietal cells. A parietal cell also contains gastrin receptors on its surface. The combination of gastrin with these receptors causes parietal cell stimulation and the production of HCl. Histamine produced by mast cells is situated very close to parietal cells. Histamine stimulates HCl secretion by stimulating histamine receptors on parietal cells.
Other notable factors influencing HCl secretion include calcium, alcohol, coffee, acidity, and food fat.
Parietal cells also contain Somatostatin and Prostaglandin receptors. Both are inhibitors of HCl secretion. Somatostatin is secreted by D cells of the gastric antral mucosa. D and G cells lie side by side and exert a paracrine effect on each other.
Epidemiology of Peptic ulcers:
A higher prevalence of peptic ulcers is in developing countries. Helicobactor Pylori is sometimes associated with socioeconomic status and poor hygiene.
According to the latest WHO data, peptic ulcer disease death in India reached 1.20% of total death. The age-adjusted death rate is 12.37 per 1,00,000 of population ranks India 5th in the world.
The mortality rate has decreased dramatically in the past 20 years.
Pathophysiology of Peptic ulcers:
The normal stomach maintains a balance between the protective factors (i.e.: mucus and bicarbonate secretion, blood flow) and aggressive factors (i.e. acid secretion, pepsin). Gastric ulcers develop when aggressive factors overcome the protective mechanism.
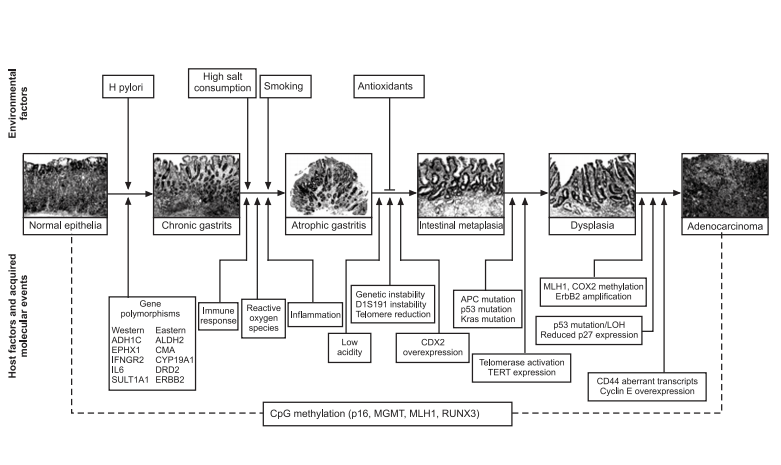
In addition to an increase in acid secretion, H. pylori also predispose patients to PUD by disrupting mucosal integrity. The bacterium’s spiral shape, flagella, and mucolytic enzymes, which it produces facilitate its passage through the mucous layer to the gastric surface epithelium. Subsequently, it releases phospholipase and proteases, which cause further mucosal damage. A cytotoxin-associated gene (cag A) has been isolated in approximately 65% of the bacteria. The products of this gene are associated with more severe gastritis, gastric ulcer, gastric cancer, and lymphoma.
NSAID-induced ulcers account for approximately 26% of gastric ulcers, and they are believed to be secondary to a decrease in prostaglandin production resulting from the inhibition of cyclooxygenase. The topical effects of NSAIDs are superficial gastric erosions and petechial lesions. However, the risk of gastroduodenal ulcer is not diminished with parental or rectal use of NSAIDs indicating injury occurring from the systemic effect of NSAIDs on the gastrointestinal mucosa. The greatest risk of developing an ulcer occurs during the first three months of NSAID use; thereafter, the risk decreases but continues to be present. Whether concurrent H pylori infection and NSAID use are synergistic in producing gastric ulcers, remains unclear.
Cigarette smoking can affect gastric mucosal defense adversely. Cigarette smoking is believed to play a facultative role in H pylori infection, that is, people who smoke tend to develop frequent and recurrent ulcers and their ulcers are more resistant to therapy.
There are two different types of peptic ulcers.
- Gastric ulcers, which form in the lining of the stomach.
- Duodenal ulcer, which forms in the upper small intestine.
Both types of peptic ulcers are most commonly caused either by infection with Helicobacter pylori bacteria or by frequent use of nonsteroidal anti-inflammatory drugs.
Clinical Manifestations:
Mild inflammation due to small ulcers may not cause any major symptoms and may heal on their own as mouth ulcers do. However, some ulcers can cause serious symptoms.
Stomach pain is the most common symptom. The type of pain can vary from mild to severe and may occur typically at night. It may become severe as the stomach empties and in some cases may be relieved after having food. In some cases, pain may disappear for a few days and then reappear.
Other less common signs include:
- Bloating,
- Heartburn,
- Nausea or vomiting.
In severe cases, symptoms can include:
- Dark or black stool (due to bleeding),
- Vomiting blood,
- Weight loss,
- Severe pain in the mid to upper abdomen.
Complications of Peptic ulcers:
Gastrointestinal bleeding is the most common complication. Sudden large bleeding can be life-threatening. It occurs when the ulcer erodes one of the blood vessels, such as the gastroduodenal artery.
Perforation (a hole in the wall of the GIT) often leads to catastrophic consequences if left untreated. Erosion of the gastro-intestinal wall by the ulcer leads to spillage of the stomach or intestinal content into the abdominal cavity. Perforation at the anterior surface of the stomach leads to acute peritonitis, initially chemical and later bacterial peritonitis.
Gastric outlet obstruction is the narrowing of the pyloric canal by scarring and swelling of the gastric antrum and duodenum due to peptic ulcers.
Cancer is included in the differential diagnosis elucidated by biopsy. Helicobacter pylori as the etiological factor make it 3 to 6 times more likely to develop stomach cancer from the ulcer.
Tests and Diagnosis:
Diagnosis mainly depends on characteristic symptoms and the severity of the ulcer. Stomach pain is usually the first signal of a peptic ulcer. Some tests will be ordered so that diagnosis can be confirmed, such as:
General Investigation:
Physical examination and recording of patient’s history.
There are no established blood tests that can reliably predict the presence of peptic ulcer disease. However, a complete blood count and blood chemistries (including liver function tests, amylase, lipase, and serum calcium levels) are generally obtained.
H. Pylori can be diagnosed by a urea breath test, blood test, stool antigen assays, and rapid urease test on a biopsy sample.
Table: Comparison of duodenal and gastric ulcers
| Duodenal Ulcers | Gastric Ulcers |
| (i) Most common in middle age and peak level is 30-50 years. | (i) Common in late middle age but incidence increases with age. |
| (ii) The male to female ratio is 4:1. | (ii) The male to female ratio is 2:1 |
| (iii) It is more common in patients with blood group O. | (iii) More common in patients with blood group A. |
| (iv) It is associated with increased serum pepsinogen. | (iv) Use of Non-steroidal anti-inflammatory drugs is associated with a three to four-fold increase in the risk of gastric ulcer |
| (v) H. pylori infection is common and seen in up to 95% of patients. In other cases, smoking is twice as common. | (iv) It is less related to H. pylori than duodenal ulcers and found in about 80% of patients. 10 – 20% of patients with a gastric ulcer have a concomitant duodenal ulcer. |
| (vi) Genetic link is more common in 1st-degree relatives. |
Blood, urea breath, and stomach tissue tests: These tests are performed to detect the presence of H. pylori. Although some of the tests for H. pylori may occasionally give false-positive results or may give false-negative results in people who have recently taken antibiotics, omeprazole, or bismuth. These tests can help detect the bacteria and guide treatment.
Radiology: Upper GI series (also called barium swallow): A diagnostic test that examines the organs of the upper part of the digestive system: the esophagus, stomach, and duodenum. A fluid called barium (a metallic, chemical, chalky, liquid used to coat the inside of organs so that they will show up on an X-ray) is swallowed. X-rays are then taken to evaluate an ulcer, scar tissue, or a blockage that is preventing food from passing through the digestive organs normally.
Endoscopy: Endoscopy is the most accurate diagnostic test for peptic ulcer disease. It involves inserting a small, lighted tube (endoscope) through the throat and into the stomach to look for abnormalities. Endoscopies are also performed if the patient has other signs or symptoms, such as weight loss, vomiting (especially if blood is present), black stools, anemia, and swallowing difficulties.
Endoscopic biopsy: During the endoscopy, a piece of stomach tissue is removed, so that it can later be analyzed for the exact cause of peptic ulcer development. This type of test is typically used for older people or those that have experienced weight loss or bleeding.
Other differential diagnoses:
- Neoplasm of the stomach,
- Pancreatitis,
- Pancreatic cancer,
- Nonulcer dyspepsia (also called functional dyspepsia),
- Cholecystitis,
- Gastritis,
- GERD – Gastroesophageal Reflux Disease,
- MI (myocardial infarction, not to be missed if having chest pain).
Treatment of Peptic ulcers:
The type of treatment is usually determined by what caused the peptic ulcer. Treatment is focused on either lowering stomach acid levels so that the ulcer can heal, or eradicating the Helicobactor pylori infection.
Treatments can include
Antibiotic medications to kill H. pylori: Antibiotic combination drug therapy regimen commonly used to treat if H. pylorus is found in the digestive tract. It likely needs to take antibiotics for two weeks, as well as additional medications to reduce stomach acid. eg. Metronidazole, Amoxycillin, tetracycline, etc.
Medications that block acid production and promote healing: Proton pump inhibitors reduce stomach acid by blocking the action of the parts of cells that produce acid and include: Omeprazole, Lansoprazole, Rabeprazole, Esomeprazole, and pantoprazole.
Medications to reduce acid production: Acid blockers, also called histamine (H2) blockers, reduce the amount of stomach acid released into the digestive tract, which relieves ulcer pain and encourages healing include: Ranitidine, Famotidine, Cimetidine, and Nizatidine.
Antacids that neutralize stomach acid: Antacids neutralize existing stomach acid and can provide rapid pain relief include: Aluminum hydroxide, Magnesium hydroxide, Calcium carbonate, and Sodium bicarbonate.
Medications that protect the lining of the stomach and small intestine: In some cases, medications called cytoprotective agents that help to protect the tissues that line the stomach and small intestine include: Sucralfate and misoprostol. Another nonprescription cytoprotective agent is bismuth sub-salicylate can also be used.
Prophylactic regimens that have been shown to dramatically reduce the risk of NSAID-induced gastric and duodenal ulcers include the use of a prostaglandin analog or proton pump inhibitors.
Surgery: In very rare cases, a complicated stomach ulcer will require surgery, especially for people who do not respond to medication, or who develop complications.
Surgery may include: Removal of the entire ulcer, taking tissue from another part of the intestines and sewing it over the ulcer site, tying off a bleeding artery, and cutting off the nerve supply to the stomach to reduce the production of stomach acid.
Vagotomy: It involves cutting the vagus nerve to interrupt messages sent from the brain to the stomach to reduce acid secretion.
Antrectomy: It involves the removing of the lower part of the stomach (antrum), which produces a hormone that stimulates the stomach to secrete digestive juices. A Vagotomy is usually done in conjunction with an antrectomy.
Pyloroplasty: Pyloroplasty is an elective surgical procedure in which the lower portion of the stomach, the pylorus, is cut and resutured, to relax the muscle and widen the opening into the small intestine, enabling contents to pass more freely from the stomach. It may be performed along with a Vagotomy.
Prevention of Peptic ulcers:
Peptic ulcers can be prevented by avoiding things that break down the stomach’s protective barrier and increase stomach acid secretion. These include alcohol, smoking, aspirin, non-steroidal anti-inflammatory drugs, and caffeine.
Preventing infection with H. pylori is a matter of avoiding contaminated food and water and adhering to strict standards of personal hygiene. Wash hands carefully with warm water and soap every time the bathroom is used, diaper changed, and before and after preparing food.
Certain lifestyle changes can reduce the risk of developing peptic ulcers by properly managing emotional and physical stress.
Make sure you also check our other amazing Article on : Alzheimer’s disease (AD)