INTRODUCTION
Table of Contents
When cells in some area of the body duplicate without control, the excess of tissue develops called tumor or neoplasm. The growth of neoplastic cells exceeds and is not coordinated with that of the normal tissues around it. The growth persists in the same excessive manner even after cessation of the stimuli. Tumors may be cancerous and sometimes fatal or they may be quite harmless. A cancerous growth is called a malignant tumor or malignancy and noncancerous growth is called benign growth. The study of tumors is called oncology.
Epidemiology:
Except for rare cases, cancer may be caused by inherited genetic defects and certain viruses. The specific cause is unknown. Several risk factors are associated with the development of cancer.
All types of cancers are common, in that, the cancer cells are abnormal and multiply out of control. However, there are often great differences between different types of cancer. For example:
- Some grow and spread more quickly than others.
- Some are easier to treat than others, particularly if diagnosed at an early stage.
- Some respond much better than others to chemotherapy, radiotherapy, or other treatments.
- Some have a better outlook (prognosis) than others. For some types of cancer, there is a very good chance of being cured. For some types of cancer, the outlook is poor.
The incidence of cancer and cancer types are influenced by many factors such as age, sex, race, local environmental factors, diet, and genetics.
Table: Risk factor and associated cancer
| Risk factor | Associated cancer |
| Male | Prostate, bladder, liver, testicle |
| Female | Breast, cervix, ovary, endometrium |
| Infection ( STD ) | Cervix, bladder |
| Hepatitis B | Liver |
| HIV | Connective tissue |
| Drug and hormone therapy Reproductive history | Bladder, skin, endometrium, breast, vagina Breast, ovary, endometrium |
| Family history | Breast, colon, lung, testicle, skin |
| Diet | Breast, colon, prostate |
| Obesity | Colon, endometrium |
| Cigarette smoking | Lung, bladder, mouth |
| Alcohol abuse | Breast, mouth, liver |
| Occupational exposure to a carcinogen | Bladder, liver, lung, skin |
| Air pollution | Lung |
| Radiation (sunlight) | Skin |
CLASSIFICATION OF CANCER
[I] Classification by Site of Origin:
By the primary site of origin, cancers may be of specific types like
- Breast cancer
- Lung cancer
- Prostate cancer
- Liver cancer
- Renal cell carcinoma (kidney cancer),
- Oral cancer
- Brain cancer etc.
[II] Classification by Tissue Types:
Based on tissue types cancers may be classified into six major categories:
- Carcinoma: This type of cancer originates from the epithelial layer of cells that form the lining of external parts of the body or the internal linings of organs within the body.
Carcinomas, malignancies of epithelial tissue, account for 80 to 90 % of all cancer cases since epithelial tissues are most abundantly found in the body from being present in the skin to the covering and lining of organs and internal passageways, such as the gastrointestinal tract. Carcinomas usually affect organs or glands capable of secretion including the breast, lungs, bladder, colon, and prostate.
2. Sarcoma: These cancers originate in connective and supportive tissues including muscles, bones, cartilage, and fat. Bone cancer is one of the sarcomas termed osteosarcoma. It affects the young most commonly. Sarcomas appear like the tissue in which they grow.
Other examples include Chondrosarcoma (of the cartilage), Leiomyosarcoma (smooth muscles), Rhabdomyosarcoma (skeletal muscles), Mesothelial sarcoma or mesothelioma (membranous lining of body cavities), Fibrosarcoma (fibrous tissue), Angiosarcoma or hemangioendothelioma (blood vessels), Liposarcoma (adipose or fatty tissue), Glioma or astrocytoma (the neurogenic connective tissue found in the brain), Myxosarcoma (primitive embryonic connective tissue) and Mesenchymous or mixed mesodermal tumor (mixed connective tissue types).
3. Myeloma: These originate in the plasma cells of bone marrow. Plasma cells are capable of producing various antibodies in response to infections. Myeloma is a type of blood cancer.
4. Leukemia: This group of cancers is grouped within blood cancers. These cancers affect the bone marrow which is the site for blood cell production. When cancerous, the bone marrow begins to produce excessive immature white blood cells that fail to perform their usual actions and the patient is often prone to infection.
Types of leukemia include:
- Acute myelocytic leukemia (AML)
- Chronic myelocytic leukemia (CML)
- Acute lymphatic, lymphocytic, or lymphoblastic leukemia (ALL)
- Chronic lymphatic, lymphocytic, or lymphoblastic leukemia (CLL)
- Polycythemia vera or erythremia
5. Lymphoma: These are cancers of the lymphatic system. Unlike the leukemias, which affect the blood and are called “liquid cancers”, lymphomas are “solid cancers”. These may affect lymph nodes at specific sites like the stomach, brain, intestines, etc. These lymphomas are referred to as extranodal lymphomas.
Lymphomas may be of two types – Hodgkin’s lymphoma and Non-Hodgkin’s lymphomas. In Hodgkin lymphoma, there is a characteristic presence of Reed-Sternberg cells in the tissue samples which are not present in Non-Hodgkin lymphoma.
6. Mixed types: These have two or more components of cancer. Some of the examples include mixed mesodermal tumor, carcinosarcoma, adenosquamous carcinoma, and teratocarcinoma. Blastomas are another type that involves embryonic tissues.
Central nervous system cancers: Cancers that begin in brain tissue or the spinal cord are known as central nervous system cancers. Primary brain tumors develop in the brain. If the tumor began in another part of the body but spread to the brain, it is called a secondary brain tumor or brain metastases. The most common type of brain tumor develops from glial cells and is called glioma.
[III] Classification by Grade:
Cancers can also be classified according to grade. The abnormality of the cells for surrounding normal tissues determines the grade of cancer. Increasing abnormality increases the grade, from 1–4.
Cells that are well differentiated closely resemble normal specialized cells and belong to low-grade tumors. Undifferentiated cells are highly abnormal for surrounding tissues. These are high-grade tumors.
- Grade 1: Well-differentiated cells with slight abnormality.
- Grade 2: Cells are moderately differentiated and slightly more abnormal.
- Grade 3: Cells are poorly differentiated and very abnormal.
- Grade 4: Cells are immature and primitive and undifferentiated.

Types of Staging:
Staging is done when a person is first diagnosed before any treatment is given. The main types of staging are:
Clinical staging: This is an estimate of the extent of cancer-based on results of physical exams, imaging tests (x-rays, CT scans, etc.), and tumor biopsies. For some cancers, the results of other tests, such as blood tests, are also used in staging.
The clinical-stage is a key part of deciding the best treatment to use. It is also the baseline used for comparison when looking at how cancer responds to treatment.
Pathologic staging: If surgery is being done, the surgeon can also determine the Pathologic stage (also called the surgical stage) of cancer. The pathologic stage relies on the results of the exams and tests mentioned before, as well as what is learned about cancer during surgery. Often this is surgery to remove cancer and nearby lymph nodes, but sometimes surgery may be done to just look at how much cancer is in the body and take out tissue samples.
Classification by Stage:
Cancer staging consists of determining the level of severity of the disease using clinical and complementary diagnostic tests. The aim is to detect the presence of visible metastases.
The most commonly used method uses classification in terms of tumor size (T), the degree of regional spread or node involvement (N), and distant metastasis (M). This is called the TNM staging.
The TNM staging system for solid tumors was developed by the Union for International Cancer Control (UICC) most commonly used in oncology.
- T stands for the original (primary) tumor.
- N stands for nodes. It tells whether cancer has spread to the nearby lymph nodes.
- M stands for metastasis. It tells whether cancer has spread to distant parts of the body.
The following chart illustrates the different types of cancer according to the tissue in which they originated.
Table: Different types of cancer according to the tissue origin
| Main types of cancer | The tissue of origin of the tumor | Frequency (estimate) | Locations |
| Adenocarcinoma | Epithelium (gland surface tissue) | 85% of all cancers | Breast, liver, kidneys, prostate, ovaries, thyroid, colon, stomach, salivary gland, lungs, etc. |
| Squamous cell carcinoma | Squamous epithelial cell (skin, mucous membranes, skin) | 85% of all cancers | Skin, gastrointestinal tract, lungs, head and neck (larynx, pharynx, oral cavity), cervix, etc. |
| Sarcoma | Supporting or musculoskeletal tissue (bone, muscle, connective and fatty tissue, etc.) | 2% of all cancers | Bone, cartilage, fatty tissue, vessels, etc. |
| Hodgkin lymphoma | B or T lymphocytes, cancer characterized by the presence of large, atypical cells | 5-7% of all cancers | Lymph nodes, spleen |
| Non-Hodgkin lymphoma | B or T lymphocytes | 5-7% of all cancers | Lymph nodes, gastrointestinal tract, skin, brain, bones, genitals, lungs, etc. |
| Leukemia | Bone marrow cells (blasts) | 4% of all cancers | Blood |
| Myeloma | Bone marrow cells (plasma cells) | 4% of all cancers | Bone marrow |
When a malignant tumor has the same name as a benign tumor, the word carcinoma or sarcoma is added to the end of the name to specify that it is cancerous.
There are exceptions: lymphoma and melanoma are always cancerous; the word “malignant” is often added to them.
Table: Typical characteristics of benign Vs malignant tumors
| Benign tumor | Malignant tumor |
| Mobile mass. | Fixed or ulcerating mass. |
| Smooth and round with a surrounding fibrous capsule. | Irregular shaped with no capsule. |
| Cells multiply slowly. | Cells multiply rapidly. |
| Histopathologically similar to tissue of origin. | Different histopathology. |
| The tumor grows by expanding and pushing away and against surrounding tissue. | The tumor grows by invading and destroying surrounding tissue. |
| Mass is mobile. | Mass is fixed. |
| Not attached to surrounding tissue. | Attached to surrounding tissue and deeply fixed in surrounding tissue. |
| Never spread to other sites. | Almost always spreads to other sites if not removed or destroyed. |
| Normal nuclei. | Abnormally large, numerous, and intensely staining nuclei. |
| Easier to remove and does not recur after excision. | Difficult to remove and recurs after excision. |
Neoplastic Cell Characteristics
- Uncontrolled proliferation
- Dedifferentiation and loss of function
- Invasiveness
- Metastasis.
Uncontrolled proliferation: Normal cell division and tissue growth occur by regulatory processes but the proliferation of cancer cells is not controlled by these processes and leads to uncontrolled proliferation which varies from type to type. Some cells slowly multiply and a few fast multiply.
Dedifferentiation and loss of function: The multiplication of normal cells in a tissue begins with the division of the undifferentiated stem cells giving rise to daughter cells. These daughter cells eventually differentiate to become the mature cells of the relevant tissue by achieving specific and characteristic physical forms, physiologic functions, and chemical properties and ready to perform their programmed functions. One of the main characteristics of cancer cells is that they dedifferentiate to varying degrees. In general, poorly differentiated cancers multiply faster and carry a worse prognosis than well-differentiated cancers.
Invasiveness: Change in the factor that regulates cell adhesion and motility (process of invading responsible for the rapid spread of cancer to a secondary site, marked by a tendency to spread especially into healthy tissue; “invasive cancer cells”).
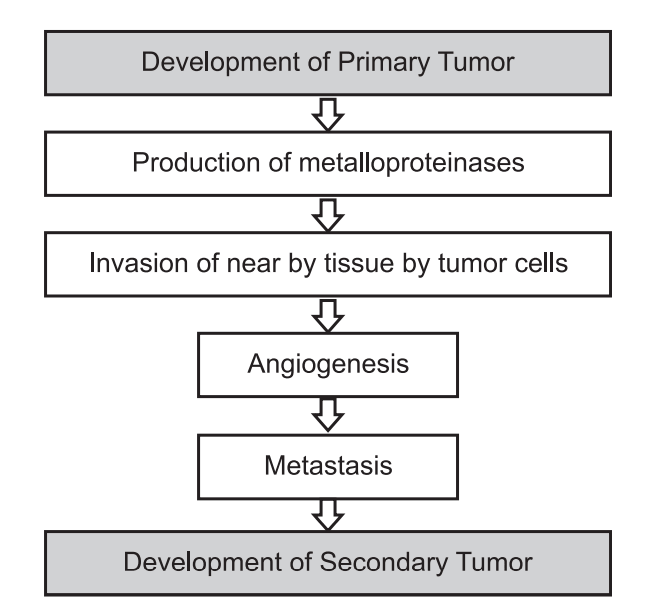
Metastasis: Migration of primary tumors to another site through blood vessels or lymphatics results in the formation of a secondary tumor.
The Genesis of A Cancer Cell:
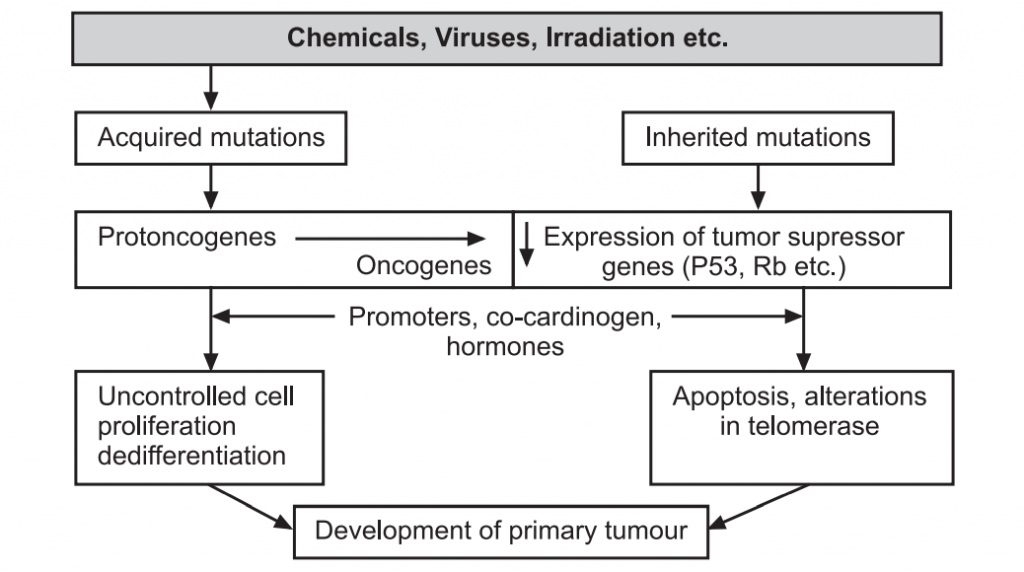
A normal cell turns into a cancer cell because of one or more mutations in its DNA, which can be inherited or acquired, usually through exposure to viruses or carcinogens (e.g. tobacco products, asbestos).
However, carcinogenesis is a complex multistage process, usually involving more than one genetic change as well as other epigenetic factors (hormonal, co[1]carcinogen and tumor promoter effects, etc.) that do not themselves produce cancer but which increase the likelihood that the genetic mutation(s) will eventually result in cancer.
There are two main categories of genetic change that are important:
- Activation of proto-oncogenes to oncogenes: Proto-oncogenes are genes that normally control cell division, apoptosis, and differentiation, but they can be converted to oncogenes that induce malignant change by viral or carcinogen action.
- Inactivation of tumor suppressor genes: Normal cells contain genes that can suppress malignant change termed tumor suppressor genes (antioncogenes) and mutations of these genes are involved in many different cancers. The loss of function of tumor suppressor genes can be a critical event in carcinogenesis.
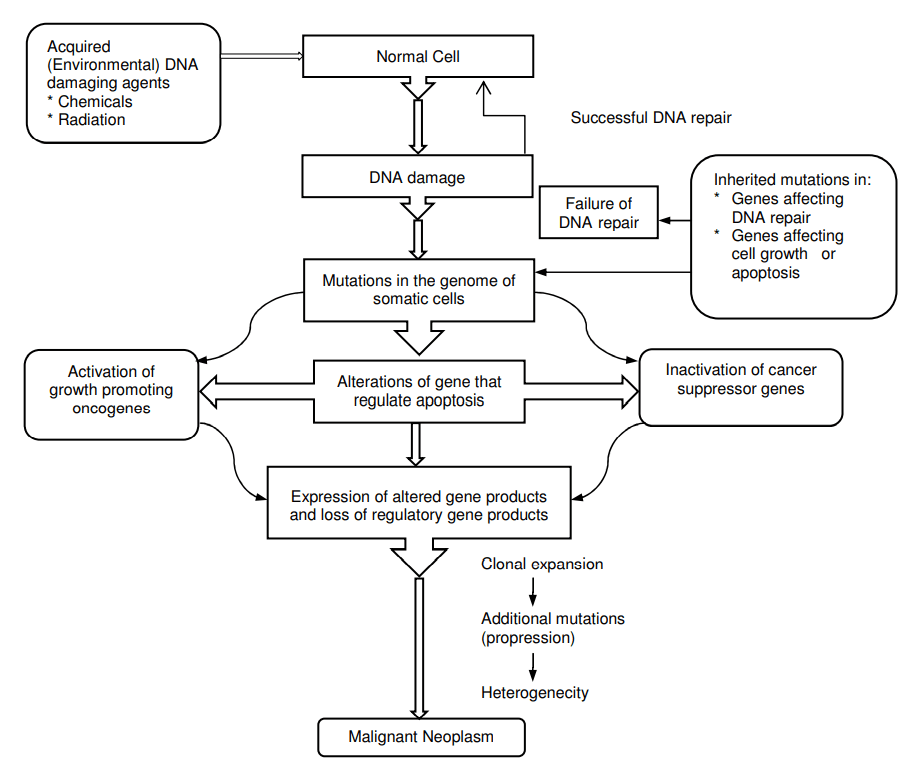
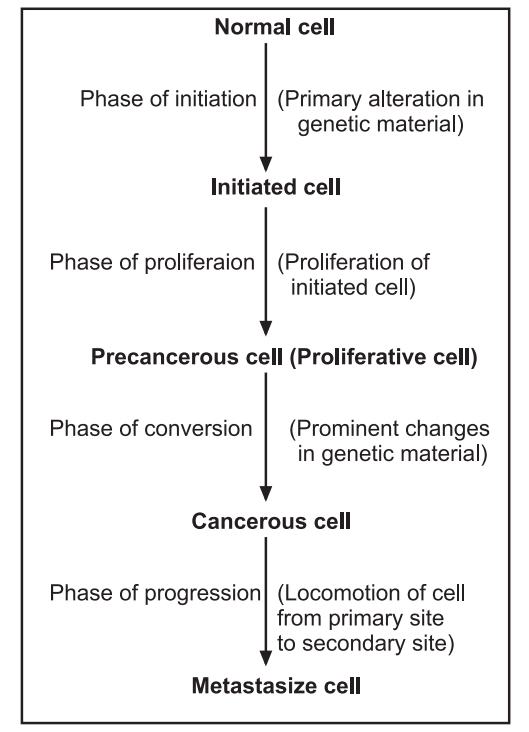
Phases of Carcinogenesis: Cancer cells develop from normal cells in a complex process consisting of four phases of transformation. These four phases convert normal cells to highly malignant cells.
ETIOLOGY:
Cancer is caused by changes (mutations) to the DNA within cells. While the underlying causes for tumor growth can vary, the process by which they grow is the same. Normally, cells in the body will naturally refresh themselves by dividing. This allows for dead cells to be disposed of naturally. In the case of tumors, dead cells may remain behind and form a growth known as a tumor. Cancer cells grow in this way as well; however, unlike the cells in benign tumors, they also invade nearby tissue. Out-of-control growth of abnormal cells causes damage to these adjacent tissues and organs and can lead to cancerous tumors in other parts of the body.
Some cancer causes remain unknown while other cancers may develop from more than one known cause. Some may be developmentally influenced by a person’s
genetic makeup. Many patients develop cancer due to a combination of these factors.
Host factor: Host factors are intrinsic to the individual patient and include age, sex, genetic factor, psychological factor, immune suppression, and chronic tissue trauma. Few cancers found in children commonly originate from embryonic tissues. In general, overall incidences increases with increase in age and are higher in man than women, maybe due to lifestyle factors rather than biological differences is susceptibility. Some cancers, such as breast, endometrial, and prostate cancers are hormonally influenced. The exact mechanism is unknown but certain psychological factors such as stress or depression increase the risk of cancer development. An increased risk of cancer has been demonstrated in patients with AIDS and those on immunosuppressive drugs, strongly suggesting a role for immunosuppression in the process of cancer development.
Environmental and lifestyle factors: Environmental and lifestyle factors include geographic location, cigarette smoking, nutrition, and occupation. Certain cancers are more prevalent in some geographic locations. The risk of developing certain cancers is increased by obesity, lack of regular exercise, drinking too much alcohol, smoking, and eating a lot of red meat. Cigarette smoking greatly increases the risk of lung cancer. About 9 out of 10 people who develop lung cancer are smokers.
A carcinogen is something (chemical, radiation, etc.) that can damage a cell and make it more likely to turn into a cancerous cell. The more exposure to a carcinogen, the greater the risk of cancer development.
Infection: Some germs (viruses and bacteria) are associated with certain cancers. hepatitis B and hepatitis C virus are usually related to hepatocellular carcinoma and have an increased risk of developing cancer of the liver. Another example is the link between human papillomavirus (HPV) and cervical cancer. Most women who develop cervical cancer have been infected with a strain of HPV at some point in their life. The relative risk of Kaposi’s sarcoma occurs in a patient with HIV infection. The Epstein Barr virus (EBV) is associated with Burkitt’s lymphoma and nasopharyngeal carcinoma. Hodgkin’s disease is also believed to be a viral origin. Another example is, Helicobactor pylori are linked to stomach cancer.
Radiation: Exposure to radioactive materials and nuclear fallout can increase the risk of leukemia and other cancers. Too much sun exposure and sunburn (radiation from UVA and UVB) increase the risk of developing skin cancer.
Genetic factors: Genetic mutation is inherited from parents. This type of mutation accounts for a small percentage of cancers. Most gene mutations occur after birth and are not inherited. Several forces can cause gene mutations, such as smoking, radiation, viruses, cancer-causing chemicals (carcinogens), obesity, hormones, chronic inflammation, and a lack of exercise.
Obscure defects: Racial predilections (American women have breast cancer more often than Japanese women; Japanese men have stomach cancer far more often than American men). However, genetic factors are less conspicuous and more difficult to identify. There is probably a complex interrelationship between heredity, susceptibility, and environmental carcinogenic stimuli in the causation of several cancers.
Age: Older persons have a greater tendency to develop neoplasm from a lack of effective control mechanisms. This is due to an accumulation of damage to cells over time. Also, the body’s defenses and resistance against abnormal cells may become less good as become older. For example, the ability to repair damaged cells and immune systems which may destroy abnormal cell may become less efficient with age.
PATHOPHYSIOLOGY:
Local Growth and Loss of Differentiation: The rate of local tumor growth is dependent on cell cycle time and rate of angiogenesis or development of blood vessels within the tumor. Epithelial cell origin tumors have a shorter cell cycle and grow rapidly than connective tissue origin. The tumor cannot enlarge beyond 1 or 2 mm in diameter, however, unless it develops its blood supply. Angiogenic cytokines that promote vessel growth are secreted by tumor cells as well as by inflammatory cells, such as macrophages, which infiltrate the area.
Initially, the cells within the malignant tumor are monoclonal or identical daughter cells of the originally mutated cells. By the time such tumors are clinically detectable, however, they have accumulated additional genetic damage. This finding is attributed to the increased risk of random mutation in cells that are dividing rapidly. Each generation of tumor cells thus becomes more poorly differentiated, bearing less resemblance in structure and function to the cell of origin.
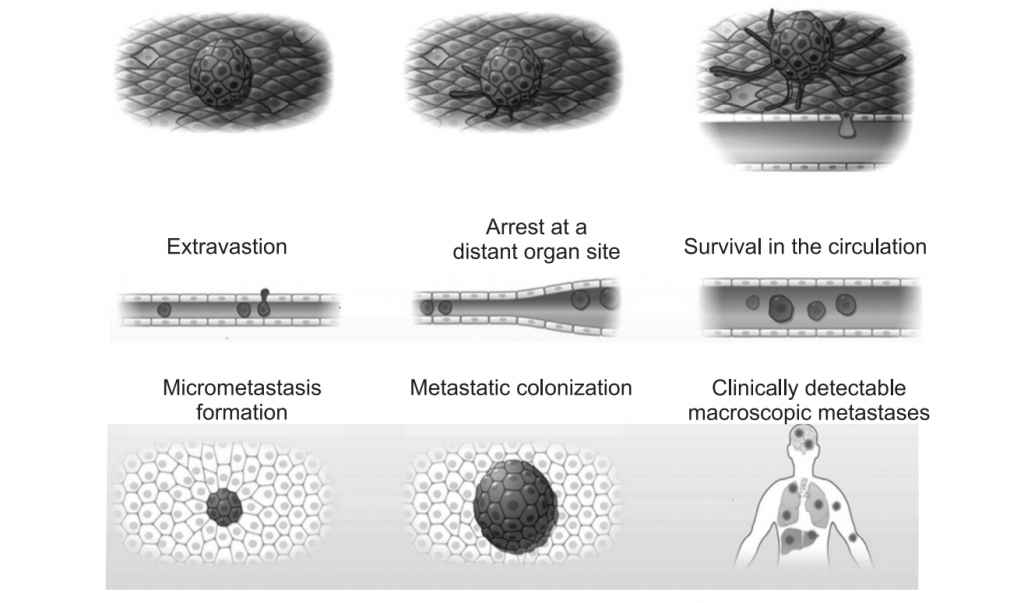
Invasion and Metastasis: Cancers typically invade tissues adjacent to the site of origin (primary site) and may metastasize to distant (secondary or metastatic) sites by mechanical or lymphatic or hematogenous (blood-born) spread.
Tumor cells within a body cavity may fall, by gravity, to lower points, establishing metastatic tumors. During surgery, manipulation of tumors may free some cells within cavities and facilitate its spread. More commonly, however, tumor cells travel in the bloodstream or lymphatic system after invasion into these channels. Cancer cells cannot metastasize unless they first separate from cells at the site of origin, invade a lymphatic or blood vessel and attach to tissues at secondary sites.
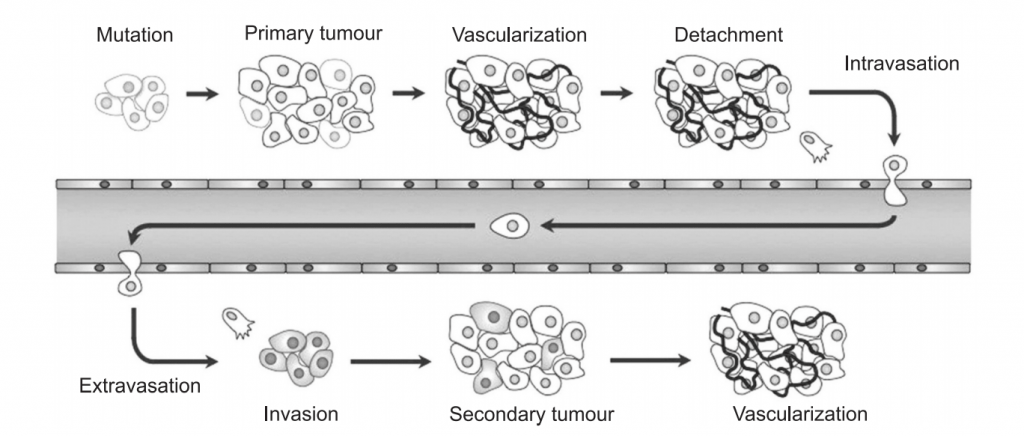
Generally, cells are held together in tissues by adhesion molecules (cadherins) is an important means of intercellular signaling. Cells that become detached are normally destroyed by apoptosis. During the process of neoplastic transformation, cancer cells may lose the ability to express these molecules, promoting detachment; other genetic alteration permits survival in the detached state.
Once detached, cancer cells must breach natural barriers before entering blood or lymphatic vessels. These barriers are the basement membranes of the tissue of origin and the vessel and the extracellular matrix between. Cancer cells, like white blood vessels, accomplish this invasion by releasing proteolytic enzymes that break down the tissue barriers. Although normal cells contain an enzyme-inhibitor system, these may be overcome, permitting local extension of the tumor and asses into the blood and lymph.
Metastasis is not inevitable once the cancer cells are in the blood or lymph. In some cases, the cells undergo apoptosis once entering these fluids. Tumor cells may be filtered out of lymph at lymph nodes, or out of blood in the spleen. Immune cells may then destroy the tumor cells at these locations. Metastatic tumors may also form at these sites or within downstream capillaries, where tumor cells become trapped because of the small vessel size.
Attachment and proliferation of cancer cells at metastatic sites depend on several factors. Usually, cancer cells in the blood become trapped within the first capillary bed downstream of their point of entry into the circulation. Blood leaving most organs first enters the capillary beds of the lungs, the most common site of metastasis. Blood from the intestine first encounters the capillary beds of the liver, and this is the second most common metastatic site. Cancer metastasis cannot always be predicted on this basis. However, some cancers appear to prefer metastatic sites other than those immediately downstream in the blood or lymphatics. Prostate cancer can spread to any part of the body, but most commonly to the bones. The reason for this selectivity resides with adhesion molecules (integrins) on the cancer cells, which bind preferentially two adhesion molecules (selectins) lining vessels within certain tissues. Secretion of hormones or growth factors by these tissues may also facilitate metastatic growth.
Symptoms:
Symptoms depend on the type and location of the tumor. For example, lung tumors may cause coughing, shortness of breath, or chest pain. Tumors of the colon can cause weight loss, diarrhea, constipation, iron deficiency anemia, and blood in the stool. Some tumors may not cause any symptoms. In certain tumors, such as pancreatic cancer, symptoms often do not start until the disease has reached an advanced stage.
Symptoms that occur with most tumors include fatigue, weight changes including unintended loss or gain, Skin changes such as yellowing, darkening or redness of the skin, changes in bowel or bladder habits, persistent cough, difficulty in swallowing, hoarseness, persistent indigestion, or discomfort after eating, persistent,
unexplained muscle or joint pain, persistent, unexplained fevers, or night sweats.
Depending on cell type, origin, location of trauma, condition of host includes:
- Malnutrition due to cytokines produced by the tumor, obstruction of GIT, anorexia, depression.
- Pain due to nerve injury related to radiation or chemotherapy.
- Infection due to immunosuppressant (barrier break down by cancer).
- Fatigue due to malnutrition, anemia, and depression.
- Bleeding due to platelet deficiency tumor production interferes with normal clotting.
- Hormonal imbalances due to inappropriate secretion of the hormone by tumor cells.
- Obstruction of hollow organs.
Cancer Diagnosis:
Like the symptoms, the signs of tumors vary based on their size and type. Some tumors are obvious, such as skin cancer. However, most cancers cannot be seen during an exam because they are deep inside the body. When a tumor is found, a biopsy is performed to determine if the tumor is noncancerous (benign) or cancerous (malignant). Depending on the location of the tumor, the biopsy may be a simple procedure or a serious operation.
Physical exam: Areas of the body for lumps that may indicate a tumor. A physical exam includes looking for abnormalities, such as changes in skin color or enlargement of an organ that may indicate the presence of cancer. A mass may be palpable or visible.
Radiographic techniques: The use of plain films (x-rays), computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET) scans, mammography, and ultrasonography (US) may be very helpful to detect the tumor type, presence, and location of mass lesions which also aid in staging and determination of therapy.
Laboratory analyses: Laboratory tests, such as urine and blood tests, may help to identify abnormalities that can be caused by cancer. For instance, in people with leukemia, a common blood test called complete blood count (CBC) may reveal an unusual number of white blood cells. Tumor markers in serum such as carcinoembryonic antigen (CEA), α-fetoprotein (AFP), or human chorionic gonadotropin (HCG) can be performed.
Genetic Testing: Genetic markers include chromosomal alterations (translocations, deletions, duplication, etc.); specific gene defects; single nucleotide polymorphisms, and gene rearrangements. Detection of specific genes (such as BRCA-1 for breast cancer) may suggest an increased risk for some malignancies.
Tissue Biopsy and Surgery: Methods that sample small pieces of tissue (biopsy) from a particular site, often via endoscopic techniques (such as colonoscopy, upper endoscopy, or bronchoscopy) can often yield a specific diagnosis of malignancy. It is also helpful to determine the stage and grade of the neoplasm.
Autopsy: The autopsy serves as a means of quality assurance for clinical diagnostic methods, as a way of confirming diagnoses helpful in establishing risks for family members, as a means for gathering statistics for decision making about how to approach diagnosis and treatment of neoplasm and to provide material for future research.
Treatment of Cancer:
Surgery: The goal of surgery is to remove cancer or as much cancer as possible. The outcome of surgery also must be acceptable to the patient in terms of quality of life issues such as disfigurement or dysfunction.
Chemotherapy: Chemotherapy uses drugs to kill cancer cells. The ideal chemotherapeutic agent would preferentially target cancer cells, by their genetic makeup, increased blood flow, or high oxygen consumption while sparing normal cells.
Radiation therapy: Radiation therapy uses high-powered energy beams, such as X-rays to kill cancer cells.
Stem cell transplant: Stem cell transplant is also known as bone marrow transplant. A stem cell transplant can use its stem cells or stem cells from a donor.
Biological therapy: Biological therapy uses the body’s immune system to fight cancer. Cancer can survive unchecked in the body because the immune system does not recognize it as an intruder. Biological therapy can help the immune system “see” cancer and attack it. Biologic response modifiers are agents that boost immune system activity or antagonize tumor growth through biological effects. These agents may be isolated from human blood, or they may be produced by recombinant DNA technology. It includes antibodies and cytokines such as interferons, interleukins, tumor necrosis factor, and colony-stimulating factors.
Hormone therapy: Some types of cancer are fuelled by the body’s hormones. Examples include breast cancer and prostate cancer. Removing those hormones from the body or blocking their effects may cause the cancer cells to stop growing.
Gene therapy: Modes of gene therapy under investigation include the use of synthetic nucleotide strands to bind defective segments of cellular DNA or mRNA. Such binding prevents the production of proteins involved in the molecular mechanism of neoplastic transformation.
Targeted drug therapy: Targeted drug treatment focuses on specific abnormalities within cancer cells that allow them to survive.
Prevention of Cancer:
Many cancers can either be prevented or the risk of developing cancers can be markedly reduced by avoiding its potential causes, public information campaigns through media, and warning labels (cigarette, tobacco, alcohol, and drug abuse). The risk of cancerous (malignant) tumors may be reduced by:
- Eating a healthy diet.
- Exercising regularly.
- Limiting alcohol.
- Maintaining a healthy weight.
- Minimizing exposure to radiation and toxic chemicals.
- Not smoking or chewing tobacco.
- Reducing sun exposure, especially if burn easily.
Make sure you also check our other amazing Article on : Gout