Introduction of Depression:
Table of Contents
Depression is a common mental disorder, characterized by sadness, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, feelings of tiredness, and poor concentration. It can be long-lasting or recurrent, substantially impairing a person’s ability to function at work or school or cope with daily life. There are many different types, caused by certain events in life and chemical changes in the brain.
Major depression: It is a presence of depressed mood or loss of pleasure for at least two consecutive weeks along with changes in appetite or weight, changes in sleep pattern, retardation, fatigue, feeling of worthlessness, excessive guilt, difficulty concentrating, and thoughts of suicide and can lead to a variety of emotional and physical problems.
Chronic major depression: Depressed mood for at least two years along with appetite disturbance, sleep disturbance, fatigue, low self-esteem, poor concentration and difficulty in making decisions, and feeling of hopelessness.
Dysthymia (recurrent, mild depression): Dysthymia is a type of chronic “low-grade”. More days than not, a person feels mildly or moderately depressed, although a person may have brief periods of normal mood.
The symptoms of dysthymia are not as strong as the symptoms of major depression, but they last a long time (at least two years). These chronic symptoms make it very difficult to live life to the fullest or to remember better times. Some people also experience major depressive episodes on top of dysthymia, a condition known as “double depression”.
Seasonal affective disorder (SAD): Some people get depressed in the fall or winter when overcast days are frequent and the sunlight is limited. This type of depression is called seasonal affective disorder (SAD). The seasonal affective disorder is more common in northern climates and younger people. Like depression, the seasonal affective disorder is treatable. Light therapy, a treatment that involves exposure to bright artificial light, often helps relieve symptoms.
Bipolar disorder: When depression is just one side of the coin, it is bipolar disorder, also known as manic depression and it is characterized by cyclic mood changes. Episodes of depression alternate with manic episodes, which can include impulsive behavior, hyperactivity, rapid speech, and little to no sleep.
Typically, the switch from one mood extreme to the other is gradual, with each manic or depressive episode lasting for at least several weeks. When depressed, a person with bipolar disorder exhibits the usual symptoms of major depression. However, the treatments for bipolar depression are very different. Antidepressants can make bipolar depression worse.
Depression affects each person in different ways; therefore symptoms caused by depression vary from person to person. Depression with specific features, such as:
Atypical features: An ability to be cheered by happy events, increased appetite, little need for sleep, sensitivity to rejection, and a heavy feeling in arms or legs.
Mixed features: Simultaneous depression and mania, which includes elevated self-esteem, talking too much, and racing thoughts and ideas.
Psychotic features: Depression accompanied by delusions or hallucinations, which may involve themes of personal inadequacy or negative themes.
Catatonia: Include a motor activity that involves either uncontrollable and purposeless movement or fixed and inflexible posture.
Peripartum onset: It occurs during pregnancy or in the weeks or months after delivery.
Epidemiology:
Depression is a major cause of morbidity worldwide. Lifetime prevalence varies widely, from 3% in Japan to 17% in the US. In most countries, the number of people who would suffer from depression during their lives falls within the 8–12% range.
In India, depression is a disorder of major public health importance, in terms of its prevalence and the suffering, dysfunction, morbidity, and economic burden. Depression is more common in women than men. It occurs in about 6% adult population because of stressful life events, prior suicidal attempts, age less than 40 years, family history of depression, recent childbirth, lack of social support, and current substance abuse.
Causes of Depression:
The causes of depression are not fully understood and may not be down to a single source. Depression is likely to be due to a complex combination of factors that include:
- Genetics
- Biological: Changes in neurotransmitter levels
- Environmental
- Psychological and social (psychosocial) Some people are at higher risk of depression than others; risk factors include:
- Life events: Including bereavement, divorce, work issues, relationships with friends and family, financial problems, medical concerns, or acute stress.
- Personality: Those with less successful coping strategies, or previous life trauma.
- Genetic factors: First-degree relatives of depressed patients are at higher risk.
- Childhood trauma.
- Some prescription drugs: Including corticosteroids, some β-blockers, interferon, and other prescription drugs.
- Abuse of recreational drugs (including alcohol and amphetamines): Can accompany depression or result in it. There are strong links between drug abuse and depression.
- A past head injury.
- People who have had an episode of major depression are at higher risk of a subsequent one.
- Chronic pain syndromes in particular, but also other chronic conditions, such as diabetes, chronic obstructive pulmonary disease, and cardiovascular disease.
Pathophysiology of Depression:
The exact pathophysiology of depression is unknown but the hypothesis is monoamine deficiency (e.g. norepinephrine and serotonin) and this may represent a final common pathway triggered by an initial disorder involving other neurotransmitters or their receptor.
Autopsy examination of neural tissue revealed that, significantly low concentration of serotonin metabolites and reduced serotonin uptake by platelet in depressed people.
Dietary restriction of L-tryptophan, an amino acid that is a serotonin precursor. Deregulation of Serotonin (5HT) and Norepinephrine (NE) in the brain is strongly associated with depression. Deregulation of 5HT and NE in the spinal cord may explain an increased pain perception among depressed patients. Decreased levels of 5HT and NE may explain the presence of both emotional and physical symptoms of depression.
Serotonin:
As a neurotransmitter, serotonin helps to relay messages from one area of the brain to another. Because of the widespread distribution of its cells, it is believed to influence a variety of psychological and other body functions. Approximately 40 million brain cells, most are influenced either directly or indirectly by serotonin.
This includes brain cells related to mood, sexual desire and function, appetite, sleep, memory and learning, temperature regulation, and some social behavior.
In terms of body function, serotonin can also affect the functioning of the cardiovascular system, muscles, and various elements in the endocrine system.
Serotonin is made via a unique biochemical conversion process. It begins with tryptophan, a building block to proteins. Cells that make serotonin use tryptophan hydroxylase, a chemical reactor that, when combined with tryptophan, forms 5-hydroxytryptamine, otherwise known as serotonin.
The link between serotonin and depression:
Researchers believe that an imbalance in serotonin levels may influence mood in a way that leads to depression. Possible problems include low brain cell production of serotonin, a lack of receptor sites able to receive the serotonin that is made, the inability of serotonin to reach the receptor sites, or a shortage in tryptophan. If any of these biochemical glitches occur, it can lead to depression.
Although it is widely believed that a serotonin deficiency plays a role in depression, there is no way to measure its levels in the living brain. Therefore, there have not been any studies proving that brain levels of this or any neurotransmitter are in short supply when depression or any mental illness develops.
Blood levels of serotonin are measurable and are lower in people who suffer from depression but researchers do not know if blood levels reflect the brain’s level of serotonin. Also, researchers do not know whether the drop in serotonin causes depression, or the depression causes serotonin levels to drop.
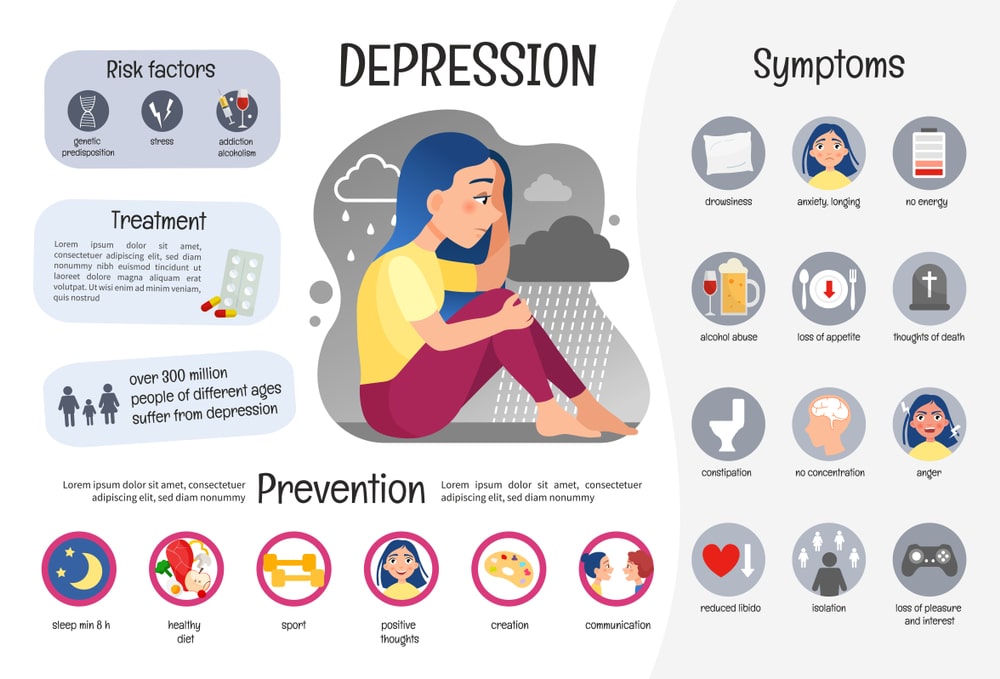
Symptoms of Depression:
People with depressive illnesses do not all experience the same symptoms. The severity, frequency, and duration of depression depending on the individual’s particular illness. Although depression may occur only one time during life, usually people have multiple episodes of depression. During these episodes, symptoms occur most of the day, nearly every day, and may include:
- Feelings of sadness, emptiness, or unhappiness.
- Angry outbursts, irritability, or frustration, even over small matters.
- Loss of interest or pleasure in normal activities, such as sex.
- Sleep disturbances, including insomnia or sleeping too much.
- Tiredness and lack of energy, so that even small tasks take extra effort.
- Changes in appetite often reduced appetite and weight loss, but increased cravings for food and weight gain in some people.
- Anxiety, agitation, or restlessness, e.g., excessive worrying, pacing, hand wringing, or an inability to sit still.
- Slowed thinking, speaking, or body movements.
- Feelings of worthlessness or guilt, fixating on past failures or blaming for the things that, they are not responsible for.
- Trouble thinking, concentrating, making decisions, and remembering things.
- Frequent thoughts of death, suicidal thoughts, suicide attempts, or suicide.
- Unexplained physical problems, such as back pain or headaches.
Symptoms in children and teens:
Common symptoms of depression in children and teens are similar to those of adults, but there can be some differences.
In younger children, symptoms of depression may include sadness, irritability, clinginess, worry, aches, and pains, refusing to go to school or being underweight.
In teens, symptoms may include sadness, irritability, feeling negative and worthless, anger, poor performance or poor attendance at school, feeling misunderstood and extremely sensitive, using drugs or alcohol, eating or sleeping too much, self-harm, loss of interest in normal activities, and avoidance of social interaction.
Depression may occur with other mental health conditions, such as anxiety, eating disorders, and substance abuse.
Symptoms in older adults:
Symptoms of depression may be different or less obvious in older adults, including Memory difficulties or personality changes, fatigue, loss of appetite, sleep problems, aches, or loss of interest in sex, which is not caused by a medical condition or medication. Often wanting to stay at home, rather than going out to socialize or doing new things, suicidal thinking or feelings, especially in older men.
It can appear as anger and discouragement, rather than feelings of sadness.
If it is very severe, there may also be psychotic symptoms, such as hallucinations and delusions.
Complications:
Depression is a serious disorder that can take a terrible toll on individuals and families. Untreated depression can result in emotional, behavioural and health problems that affect every area of life. Complications associated with depression may include:
- Excess weight or obesity, which can lead to heart disease and diabetes.
- Alcohol or substance abuse.
- Anxiety, panic disorder, or social phobia.
- Family conflicts, relationship difficulties, and work or school problems.
- Social isolation.
- Suicidal feelings, suicide attempts, or suicide.
- Premature death from other medical conditions.
Tests and Diagnosis:
These exams and tests can help to rule out other problems that could be causing symptoms, pinpoint a diagnosis and check for any related complications:
Physical examination: There are no definitive findings of depression on physical examination, although most patients will have a depressed affect, as well as a downcast gaze, furrowed brow, psychomotor slowing, speech latency, and expressions of guilt or self-blame. The physical examination and cognitive screening may be useful in ruling out common conditions that are often confused with depression (i.e., hypothyroidism, dementia) and in looking for commonly co-occurring illnesses (i.e., obesity, cancer, stroke). In some cases, depression may be linked to an underlying physical health problem.
Lab tests: Simple laboratory tests should be performed in the workup to exclude other causes of depression symptoms. Adults diagnosed with depression and with negative findings on physical examination do not routinely need further testing. Certain lab tests include a complete blood count, basic metabolic panel, and thyroid function tests to rule out anemia and thyroid disease and to assess general nutritional status.
Psychological evaluation: To check for signs of depression, the mental health provider asks about symptoms, thoughts, feelings, and behavior patterns.
Other tests may include:
• CT scan or MRI of the brain to rule out serious illnesses such as a brain tumor.
• Electrocardiogram (ECG), which is used to diagnose some heart problems.
• Electroencephalogram (EEG), which is used for recording the electrical activity of the brain.
Treatments And Drugs of Depression:
Numerous depression treatments are available. Medications and psychological counseling (psychotherapy) or other mental health counselor are very effective for most people.
Medications: Many types of antidepressant medications are available to treat it, including those below. The more commonly used medications are from the following classes:
- Selective serotonin reuptake inhibitors (SSRIs): SSRIs include Fluoxetine, Paroxetine, Sertraline, Citalopram, and Escitalopram.
- Serotonin-norepinephrine reuptake inhibitors (SNRIs): SNRI medications include Duloxetine, Venlafaxine, and Desvenlafaxine.
- Atypical antidepressants: Trazodone and Mirtazapine
- Serotonin modulators. Older, less commonly used, antidepressants include:
- Tricyclic antidepressants: Tricyclic antidepressants such as Imipramine and Nortriptyline tend to cause more severe side effects than do newer antidepressants.
- Monoamine oxidase inhibitors (MAOIs): Commonly used MAOIs are Tranylcypromine and Phenelzine. Taking MAOIs should avoid or limit certain foods, which can interact with the medication and cause serious health problems.
Psychotherapy:
Psychotherapy treatment is focused on improving positive changes in depressive patients. Many specific types of psychotherapy are used to treat depression. Each works in a slightly different way, but all have been proven to help improve the symptoms of depression.
- Cognitive-behavioral therapy (CBT): In CBT, the therapist is to identify and reshape the thought and behavior patterns that contribute to depression.
- Interpersonal psychotherapy: In interpersonal psychotherapy, the focus is on the improvement of relationships, the way that depressive patients interact with other people in their life.
- Family and couples therapy: In family and couples therapy, the therapist shall improve the interaction of the patient with family members so that depressive patients can work together on the issues that are contributing to depression.
- Problem-solving therapy: In problem-solving therapy, the therapist has to develop a practical and systematic approach to the problems in life and find effective ways to solve them.
- Psychodynamic psychotherapy: In psychodynamic therapy, the therapist might explore childhood or historic life events and work to reduce their influence by gaining insight into how they may be shaping current behavior.
Prevention:
Avoid alcohol drinking or the use of illegal drugs. These substances can make depression worse and might lead to thoughts of suicide. Take the medication exactly as instructed.
There is no sure way to prevent depression. However, the following strategies may help feel better:
Get more exercise, maintain good sleep habits, seek out activities that bring pleasure, volunteer or get involved in group activities, try to be around people who are caring and positive, intervening with a depressed friend, be empathetic and understanding, avoid critical or shaming statements and challenge expressions of hopelessness.
Make sure you also check our other amazing Article on : Stroke