Introduction of Emphysema:
Table of Contents
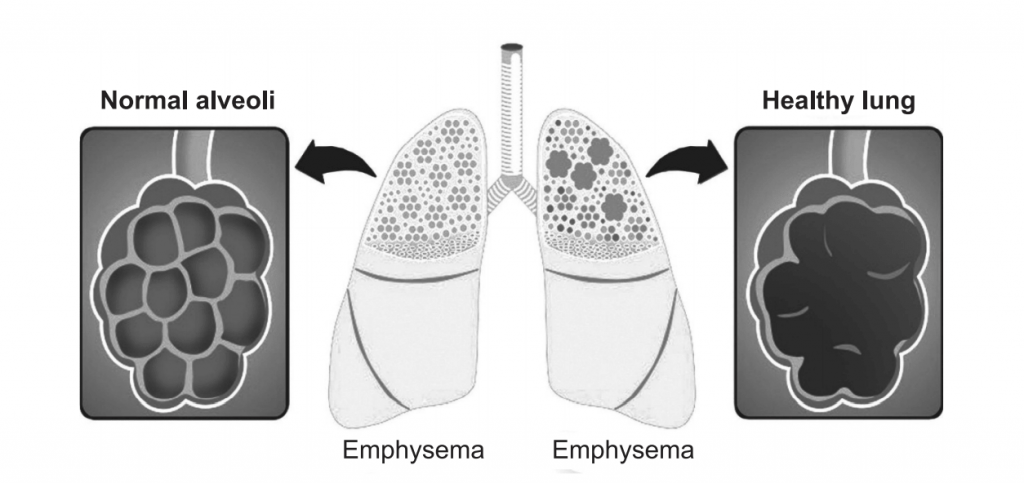
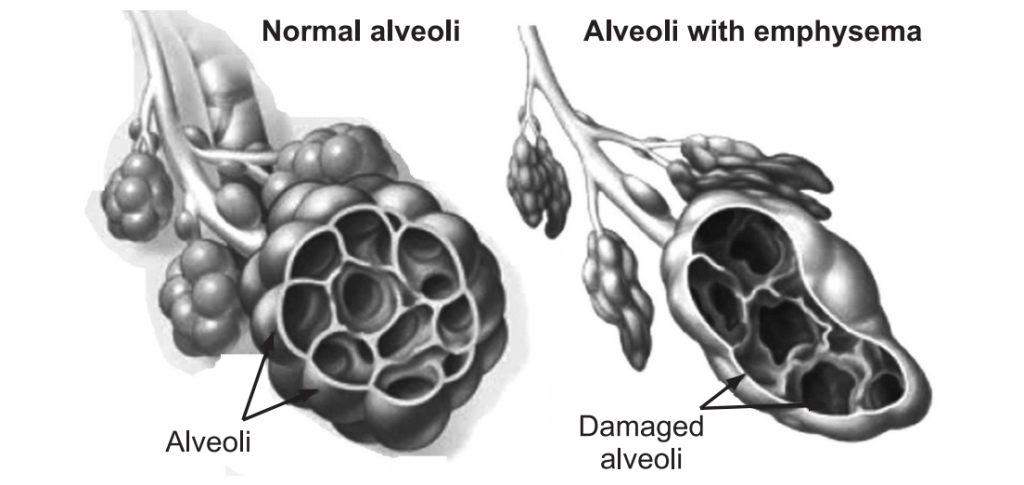
Emphysema is a long-term, progressive disease of the lungs that primarily causes shortness of breath due to over-inflation of the alveoli (air sacs in the lung). In people with emphysema, the lung tissues involved in the exchange of gases (oxygen and carbon dioxide) are impaired or destroyed. It is included in a group of diseases called chronic obstructive pulmonary disease or COPD. Emphysema is called an obstructive lung disease because the destruction of lung tissue around smaller airways (bronchioles), makes these airways unable to hold their shape properly when exhale. This makes them inefficient at transferring oxygen into the blood, and in taking carbon dioxide out of the blood.
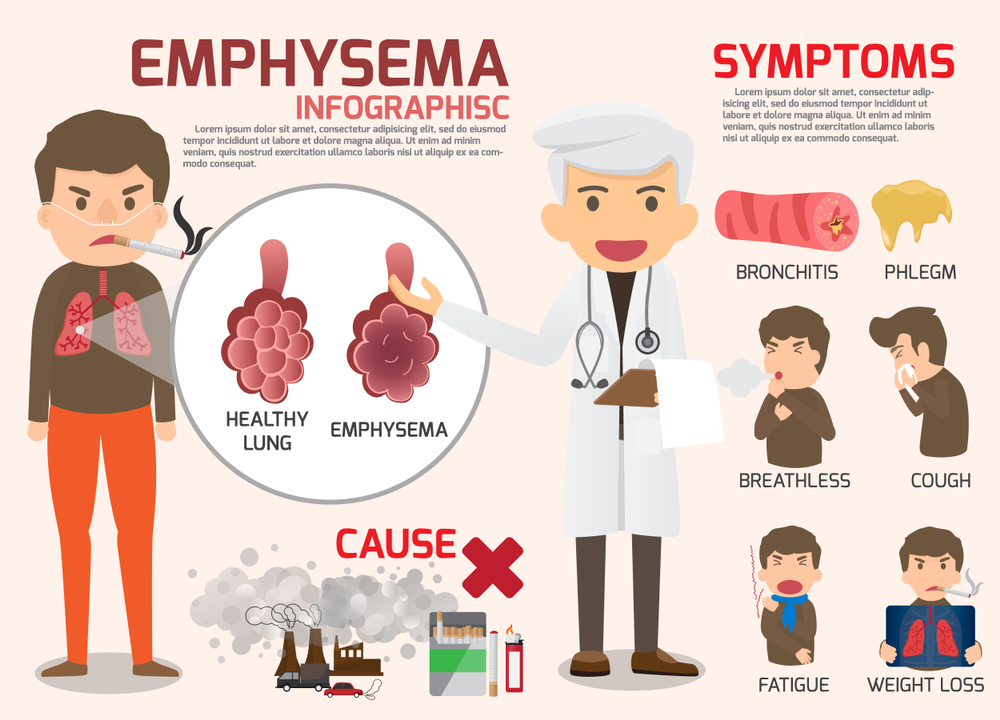
Causes of Emphysema:
The main cause of emphysema is long-term exposure to airborne irritants, including:
- Tobacco smoke
- Marijuana smoke
- Air pollution
- Chemical fumes and dust
Cigarette smoking is by far the most dangerous behavior that causes people to develop emphysema, and it is also the most preventable cause. Other risk factors include a deficiency of an enzyme called α-1- antitrypsin, air pollution, airway reactivity, heredity, male sex, and age.
The importance of cigarette smoking as a risk factor for developing emphysema cannot be overemphasized. Cigarette smoke contributes to this disease process in two ways. It destroys lung tissue, which results in the obstruction of airflow, and it causes inflammation and irritation of airways that can add to airflow obstruction.
- Destruction of lung tissue occurs in several ways. First, cigarette smoke directly affects the cells in the airway responsible for clearing mucus and other secretions. Occasional smoking temporarily disrupts the sweeping action of tiny hairs called cilia that line the airways. Continued smoking leads to longer dysfunction of the cilia. Long-term exposure to cigarette smoke causes the cilia to disappear from the cells lining the air passages. Without the constant sweeping motion of the cilia, mucous secretions cannot be cleared from the lower respiratory tract. Furthermore, smoke causes mucous secretion to be increased, at the same time that the ability to clear the secretions is decreased. The resulting mucous deposition can provide bacteria and other organisms with a rich source of food and lead to infection.
- The immune cells in the lung, whose job is to prevent and fight infection, are also affected by cigarette smoke. They cannot fight bacteria as effectively, or clear the lungs of the many particles (such as tar) that cigarette smoke contains. In these ways, cigarette smoke sets the stage for frequent lung infections. Although these infections may not even be serious enough to require medical care, the inflammation caused by the immune system constantly attacking bacteria or tar leads to the release of destructive enzymes from the immune cells.
- Over time, enzymes released during this persistent inflammation lead to the loss of proteins responsible for keeping the lungs elastic. In addition, the tissue separating the air cells (alveoli) from one another also is destroyed. Over years of chronic exposure to cigarette smoke, the decreased elasticity and destruction of alveoli leads to the slow destruction of lung function.
- Air pollution acts similarly to cigarette smoke. The pollutants cause inflammation in the airways, leading to lung tissue destruction.
- Close relatives of people with emphysema are more likely to develop the disease themselves. This is probably because the tissue sensitivity or response to smoke and other irritants may be inherited. The role of genetics in the development of emphysema, however, remains unclear.
- Abnormal airway reactivity, such as bronchial asthma, is a risk factor for the development of emphysema.
- Men are more likely to develop emphysema than women. The exact reason for this is unknown, but differences between male and female hormones are suspected.
- Older age is a risk factor for emphysema. Lung function normally declines with age. Therefore, it is the reason that the older the person, the more likely they will have enough lung tissue destruction to produce emphysema.
Rarely, emphysema is caused by an inherited deficiency of a protein that protects the elastic structures in the lungs. It is called α-1-antitrypsin deficiency emphysema.
α-1-antitrypsin deficiency:
α-1-antitrypsin (also known as α-1- antiprotease) AAT is a glycoprotein member of the serine protease inhibitor family that is synthesized in the liver and is secreted into the bloodstream. It is a substance that fights a destructive enzyme in the lungs called trypsin (or protease). Trypsin is a digestive enzyme, most often found in the digestive tract, where it is used to help the body digest food. It is also released by immune cells in their attempt to destroy bacteria and other materials. People with an α-1-antitrypsin deficiency cannot fight the destructive effects of trypsin once it is released in the lung. The destruction of tissue by trypsin produces similar effects to those seen with cigarette smoking. The lung tissue is slowly destroyed, thus decreasing the ability of the lungs to perform appropriately. Foreign objects (e.g. bacteria) are trying to be destroyed but this enzyme destroys normal tissue since the second enzyme (antiprotease) responsible for controlling the first enzyme (protease) is not available or is poorly functioning. This is referred to as the “Dutch” hypothesis of emphysema formation.
The American Thoracic Society/ European Respiratory Society Guidelines recommend screening for AAT deficiency if emphysema is suspected in any patient younger than 45 years and with any of the following:
- Absence of recognized emphysema, risk factors such as smoking, or occupational inhalational exposure.
- Unexplained liver disease.
- Family history of AAT deficiency, COPD, bronchiectasis, or panniculitis.
- Positive c-ANCA (anti-neutrophilic cytoplasmic antibody) vasculitis.
- Unclear/idiopathic bronchiectasis.
- Asthma with persistent, fixed-airways obstruction despite therapy.
Risk Factors of Emphysema:
Factors that increase the risk of developing emphysema include:
- Smoking: Emphysema is most likely to develop in cigarette smokers, but cigar and pipe smokers also are susceptible. The risk for all types of smokers increases with the number of years and amount of tobacco smoked.
- Age: The lung damage that occurs in emphysema develops gradually; most people with tobacco-related emphysema begin to experience symptoms of the disease between the ages of 40 and 60.
- Exposure to second-hand smoke: Second-hand smoke, also known as passive or environmental tobacco smoke, is smoke that you inadvertently inhale from someone else’s cigarette, pipe, or cigar. Being around second-hand smoke increases your risk of emphysema.
- Occupational exposure to fumes or dust: Breathe fumes from certain chemicals or dust from grain, cotton, wood, or mining products, are more likely to develop emphysema. This risk is even greater in cigarette smokers.
- Exposure to indoor and outdoor pollution: Breathing indoor pollutants, such as fumes from heating fuel, as well as outdoor pollutants, car exhaust, for instance, increases the risk of emphysema.
Symptoms of Emphysema:
Two of the key symptoms of emphysema are shortness of breath and a chronic cough appears in the early stages. A person with shortness of breath, or dyspnea, feels being unable to catch a breath may start only during physical exertion, but as the disease progresses, it can start to happen during rest, too.
Emphysema and COPD develop over several years.
In the later stages, the person may have:
- Frequent lung infections,
- Excess production of mucus,
- Wheezing,
- Reduced appetite and weight loss,
- Fatigue,
- Blue-tinged lips or fingernail beds, or cyanosis, due to a lack of oxygen,
- Anxiety and depression,
- Sleep problems,
- Morning headaches due to a lack of oxygen, when breathing at night is difficult.
Complications:
People who have emphysema are also more likely to develop:
• Collapsed lung (pneumothorax): A collapsed lung can be life-threatening in people who have severe emphysema because the function of their lungs is already so compromised. This is uncommon but serious when it occurs.
• Heart problems: Emphysema can increase the pressure in the arteries that connect the heart and lungs. This can cause a condition called corpulmonale, in which a section of the heart expands and weakens.
• Large holes in the lungs: Some people with emphysema develop empty spaces in the lungs called bullae. They can be as large as half the lung. In addition to reducing the amount of space available for the lung to expand, giant bullae can increase your risk of pneumothorax.
Tests and Diagnosis:
Diagnosis will carry out a physical examination and ask the patient about their symptoms and medical history. Some diagnostic tests may also be used, to confirm that the patient has emphysema rather than asthma and heart failure. If the patient has never smoked; a test may be carried out to see if the person has an α1- antitrypsin deficiency.
- A chest X-ray helps to identify changes in the lung that may indicate emphysema. The X-ray also may show the presence of an infection or a mass in the lung (such as a tumor) that could explain symptoms. Shortness of breath has many causes. The chest X-ray is considered to be the quickest and easiest test to begin to separate the different possible causes and formulate a diagnosis.
- Lung function tests can give specific information about how the lungs work mechanically. In these tests, the patient has to breathe into a tube that is connected to a computer or some other monitoring device, which can record the necessary information. The tests measure how much air in the lungs can hold, how quickly lungs can expel air during expiration, and how much reserve capacity of lungs have for increased demand, such as during exercise.
- A blood test is used to detect a family history of α1-antitrypsin deficiency to evaluate genetic disease.
- Blood tests may also be used to check white blood cell count, which can sometimes indicate an acute infection. This information can be used with the chest X-ray to evaluate for pneumonia, bronchitis, or other respiratory infections that can make emphysema worse.
- Another blood test that may be helpful, especially in the hospital setting, is called arterial blood gas. This test helps determine how much oxygen and carbon dioxide are in the blood.
Treatment of Emphysema:
Treatment for emphysema can take many forms in a step-wise approach, depending on the severity of the condition.
Medications used for the treatment of emphysema are:
Bronchodilator: Salmeterol, Albuterol, Metaproterenol, and Formoterol
Anticholinergic: Ipratropium bromide and Tiotropium
Steroids: Prednisone, Dexamethasone
PDE4 inhibitors: Roflumilast
Stop smoking: This recommendation for people with emphysema, quitting smoking may halt the progression of the disease and improve the function of the lungs to some extent. Lung function deteriorates with age. In those susceptible to developing COPD, smoking can result in a five-fold deterioration of lung function. Smoking cessation may return lung function from this rapid deterioration to its normal rate after smoking is stopped.
Antibiotics: These medications are often prescribed for people with emphysema who have increased shortness of breath. Even when the chest X-ray does not show pneumonia or evidence of infection, people treated with antibiotics tend to have shorter episodes of shortness of breath. It is suspected that infection may play a role in an acute bout of emphysema, even before the infection worsens into pneumonia or acute bronchitis.
Oxygen Therapy: As a patients’ disease progresses, they may find it increasingly difficult to breathe on their own and may require supplemental oxygen.
Surgery: People with severe emphysema sometimes undergo surgery to reduce lung volume or carry out lung transplantation. Lung volume reduction surgery removes small wedges of the damaged, emphysematous, lung tissue. This is thought to enhance lung recoil and to improve the function of the diaphragm. In severe cases, this can improve lung function, exercise tolerance, and quality of life.
Lung transplantation improves the quality of life, but not life expectancy, for people with severe emphysema. Lifelong drug therapy is necessary to prevent the immune system from rejecting the new tissue. One or both lungs may be transplanted.
Make sure you also check our other amazing Article on : Bronchitis