Introduction of Hypertension:
Table of Contents
Hypertension is a chronic medical condition that arises when the blood pressure is abnormally high (greater than 140 mm of Hg systolic and 90 mm of Hg diastolic). Hypertension occurs when the body’s smaller blood vessels (the arterioles) narrow, causing the blood to exert excessive pressure against the vessel walls and forcing the heart to work harder to maintain the pressure. Although the heart and blood vessels can tolerate increased blood pressure for months and even years, eventually the heart may enlarge (a condition called hypertrophy) and be weakened to the point of failure.
Hypertension risk factors include obesity, drinking too much alcohol, smoking, and family history.
Blood pressure is a measure of two pressures, the systolic and the diastolic. Systolic pressure is the force that blood exerts on the artery walls as the heart contracts to pump the blood to the peripheral organs and tissues. The diastolic pressure is residual pressure exerted on the arteries as the heart relaxes between beats. A diagnosis of hypertension is made when blood pressure reaches or exceeds 140/90 mmHg (read as “140 over 90 millimeters of mercury”).
Types of Hypertension:
There are two major types of hypertension and four less frequently found types.
Primary (Essential) Hypertension:
About 95% of people with high blood pressure have essential hypertension or primary hypertension. This condition has no identifiable medical cause. Elevated blood pressure usually begins to appear between age 30 and 50, but can begin at older ages. Usually, people with essential hypertension have no symptoms but may experience frequent headaches, tiredness, dizziness, or nose bleeds. Although the cause is unknown, contributing factors for essential hypertension may be, obesity, smoking, alcohol, diet, and inherited.
Secondary Hypertension:
About 5%-10% of people with high blood pressure have secondary hypertension. This condition has a definite cause; the most common cause of secondary hypertension is an abnormality in the arteries supplying blood to the kidneys. Other causes include airway obstruction during sleep, diseases and tumors of the adrenal glands, hormone abnormalities, thyroid disease, and too much salt or alcohol in the diet. Drugs can cause secondary hypertension, including OTC medications such as ibuprofen and pseudoephedrine.
Table: Classification of severity of hypertension
| Stage | Systolic (mm Hg) | Diastolic (mm Hg) |
| None | <130 | <85 |
| None or very mild | 130-139 | 85-89 |
| Mild | 140-159 | 90-99 |
| Moderate | 160-179 | 100-109 |
| Severe | 180-209 | 110-119 |
| Very severe | 210 or greater | 120 or greater |
Isolated Systolic Hypertension:
In this case, the systolic blood pressure (the top number) is consistently above 160 mm Hg and the diastolic below 90 mmHg. This may occur in older people and results from the age-related stiffening of the arteries. The loss of elasticity in arteries, like the aorta, is mostly due to arteriosclerosis. The Western lifestyle and diet are believed to be the root cause.
Malignant hypertension:
Malignant hypertension is the most threatening form of high blood pressure. It is marked by an unusually sudden rise in blood pressure to dangerous levels. Diastolic pressure often reaches 130 mm Hg or higher. However, malignant hypertension may also occur at lower, less alarming levels, if the rise is particularly sudden. Unlike other kinds of high blood pressure, malignant hypertension is usually accompanied by dramatic symptoms such as severe headache, shortness of breath, chest pain, nausea and vomiting, blurred vision, or even blindness, seizures, and loss of consciousness.
Malignant hypertension is an emergency condition. Patients with malignant hypertension must be hospitalized immediately. It places people at immediate risk for heart attack, stroke, heart failure, permanent kidney damage, bleeding into the brain (hemorrhagic stroke), and brain swelling.
Malignant hypertension develops in less than 1 % of people who already have high blood pressure. Rarely, the appearance of malignant hypertension is the first sign that a person has high blood pressure. The cause of this condition is usually unknown, but occasionally it can be a reaction of the body to drug abuse, like cocaine, or a reaction to stopping a blood-pressure medicine.
Resistant Hypertension:
If blood pressure cannot be reduced to below 140/90 mmHg, despite a triple-drug regimen of antihypertensive medications called resistant hypertension.
Resistant hypertension may occur in 20 to 30 % of high blood pressure cases. It may have a genetic component and is more common in people who are older, obese, and female or have an underlying illness, such as diabetes or kidney disease.
Hypertension during Pregnancy:
High blood pressure occurs in 6 % to 8 % of pregnancies, and in most of these cases, it is diagnosed during the first pregnancy. Pregnancy can cause high blood pressure due to hormonal changes or from a serious complication of pregnancy known as preeclampsia, a condition that causes tightening of arteries throughout the mother’s body and placenta, as well as unpredictable blood clotting.
Epidemiology of Hypertension:
As per the World Health Statistics 2012, of the estimated 57 million global deaths in 2008, 36 million (63%) were due to non-communicable diseases (NCDs). The largest proportion of NCD deaths is caused by cardiovascular diseases (48%). In terms of attributable deaths, raised blood pressure is one of the leading behavioral and physiological risk factors to which 13% of global deaths are attributed. Hypertension is reported to be the fourth contributor to premature death in developed countries and the seventh in developing countries. Recent reports indicate that nearly 1 billion adults (more than a quarter of the world’s population) had hypertension in 2000, and this is predicted to increase to 1.56 billion by 2025. Earlier reports also suggest that the prevalence of hypertension is rapidly increasing in developing countries and is one of the leading causes of death and disability.
Children:
Most childhood hypertension, particularly in preadolescents, is secondary to an underlying disorder. Apart from obesity, kidney disease is the most common (60–70%) cause of hypertension in children. Adolescents usually have primary (essential) hypertension, which accounts for 85–95% of cases.
Etiology of Hypertension:
The exact causes of high blood pressure are not known, but several factors and conditions may play a role in its development, including:
• Smoking
• Being overweight or obese
• Lack of physical activity
• Too much salt in the diet
• Too much alcohol consumption
• Stress
• People with family members who have high blood pressure
• Chronic renal failure
• Adrenal and thyroid disorders
Many people with kidney disorders have secondary hypertension. The kidneys regulate the balance of salt and water in the body if the kidneys cannot rid the body of excess salt and water, blood pressure goes up.
Kidney infections, a narrowing of the arteries that carry blood to the kidneys, called renal artery stenosis and other kidney disorders can disturb the salt and water balance.
Cushing’s syndrome and tumors of the pituitary and adrenal glands often increase levels of the adrenal gland hormones like cortisol, adrenaline, and aldosterone, which can cause hypertension.
Certain medications, such as birth control pills, cold remedies, decongestants, over-the-counter pain relievers, and some prescription drugs, illegal drugs, such as cocaine and amphetamines or chronic alcohol use, obstructive sleep apnea, and pregnancy may lead to hypertension.
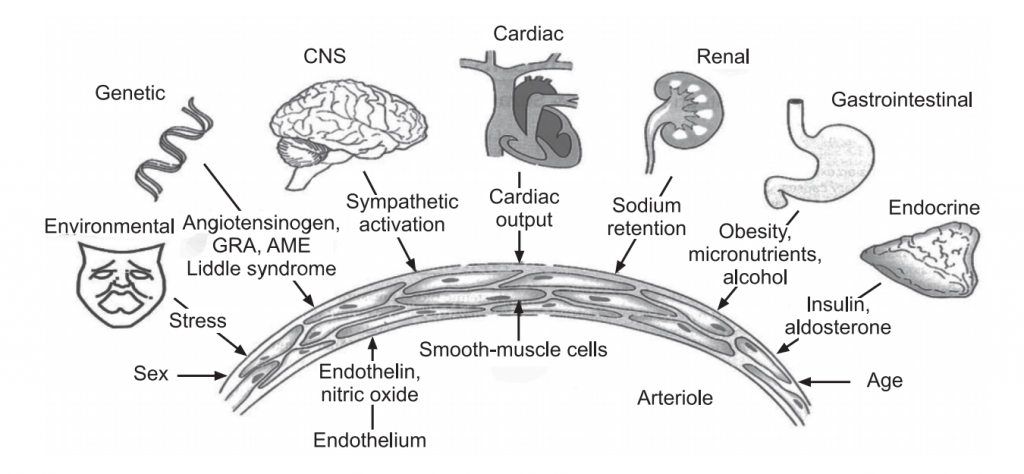
Pathophysiology of Hypertension:
Hypertension causes three major circulatory abnormalities: increased arteriolar resistance increased large artery stiffness and early or premature reflection of arterial pulse waves.
Increased resistance and vessel stiffness in younger hypertensive patients result from structural changes, including thinning and fracturing of elastin, increased collagen deposition, and increased wall thickness. These changes manifest primarily as a greater rise in systolic pressure greater than diastolic pressure.
In the elderly, andd increased arterial stiffness is the greater factor and may contribute to isolated systolic hypertension, in which systolic pressure is elevated but diastolic pressure is normal or low. Patients with isolated systolic hypertension are at substantially increased risk for stroke, coronary heart disease, and congestive heart failure. Pulse wave reflection refers to the backward rebound of some of the cardiac output as it encounters the resistance of the arteries. When arteries are normally complaint, this reflected flow occurs during diastole and assists with a filling of the coronary arteries. In hypertension, however, reflection occurs prematurely, during systole, contributing to vascular overload in the aortic arch the coronary carotid, and renal arteries.
Secondary hypertension accounts for approximately 5-10% of all cases of hypertension, with the remaining being primary hypertension. Secondary hypertension has an identifiable cause whereas primary hypertension has no known cause (i.e. idiopathic).
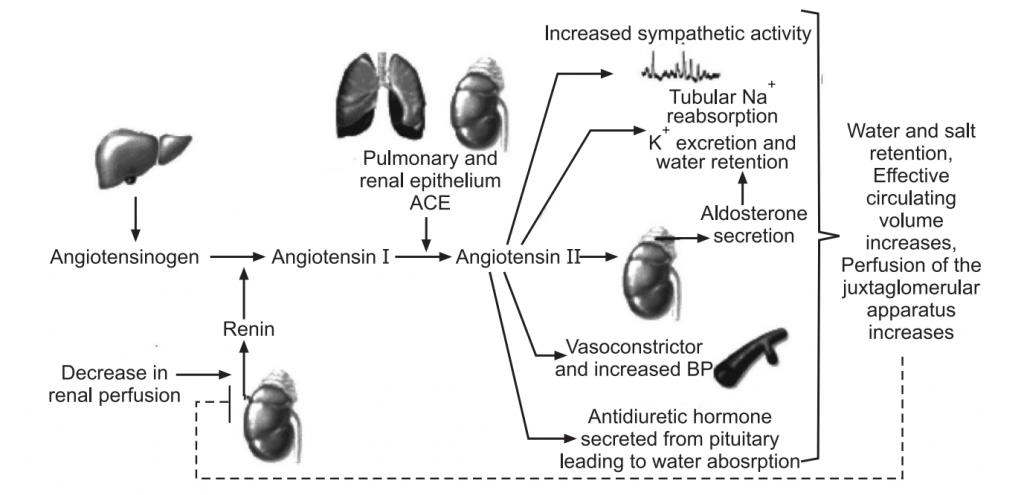
Many known conditions can cause secondary hypertension. Regardless of the cause, arterial pressure becomes elevated either due to an increase in cardiac output, an increase in systemic vascular resistance, or both. When cardiac output is elevated, it is generally due to either increased neurohumoral activation of the heart or increased blood. Increased systemic vascular resistance is most commonly caused, at least initially, by increased sympathetic activation or by the effects of circulating vasoconstrictors (e.g., angiotensin II). Anatomic considerations, such as narrowing of the aorta (e.g., coarctation) or chronic changes in vascular structure (e.g., vascular hypertrophy) can also cause or contribute to increased systemic vascular resistance. Renal artery disease can cause narrowing of the vessel lumen (stenosis). The reduced lumen diameter decreases the pressure at the afferent arteriole in the kidney and reduces renal perfusion. This stimulates renin release by the kidney, which increases circulating angiotensin II and aldosterone. These hormones increase blood volume by enhancing renal reabsorption of sodium and water. Increased angiotensin II also causes systemic vasoconstriction and enhances sympathetic activity. Chronic elevation of angiotensin II promotes cardiac and vascular hypertrophy. The net effect of these renal mechanisms is an increase in blood volume that augments cardiac output.
Therefore, hypertension caused by renal artery stenosis results from both an increase in systemic vascular resistance and an increase in cardiac output.
Chronic renal failure:
Several pathologic processes (e.g., diabetic nephropathy, glomerulonephritis) can damage nephrons in the kidney. When this occurs, the kidney cannot excrete a normal amount of sodium which leads to sodium and water retention, increased blood volume, and increased cardiac output by the Frank-Starling mechanism.
Renal disease may also result in increased release of renin leading to a renin-dependent form of hypertension. The elevation in arterial pressure secondary to renal disease can be viewed as an attempt by the kidney to increase renal perfusion and restore glomerular filtration.
Primary hyperaldosteronism:
Increased secretion of aldosterone generally results from adrenal adenoma or adrenal hyperplasia. Increased circulating aldosterone causes renal retention of sodium and water, so blood volume and arterial pressure increase. Plasma renin levels are generally decreased as the body attempts to suppress the renin-angiotensin system; there is also hypokalemia associated with the high levels of aldosterone.
Stress:
Emotional stress leads to activation of the sympathetic nervous system, which causes increased release of norepinephrine from sympathetic nerves in the heart and blood vessels, leading to increased cardiac output and increased systemic vascular resistance. Furthermore, the adrenal medulla secretes more catecholamines (epinephrine and norepinephrine). Activation of the sympathetic nervous system increases circulating angiotensin II, aldosterone, and vasopressin, which can increase systemic vascular resistance. Prolonged elevation of angiotensin II and catecholamines can lead to cardiac and vascular hypertrophy, both of which can contribute to a sustained increase in blood pressure.
Sleep Apnea:
Sleep apnea is a disorder in which people repeatedly stop breathing for short periods (10-30 seconds) during their sleep. This condition is often associated with obesity, although it can have other causes such as airway obstruction or disorders of the central nervous system. These individuals have a higher incidence of hypertension. The mechanism of hypertension may be related to sympathetic activation and hormonal changes associated with repeated periods of apnea-induced hypoxia and hypercapnia, and from stress associated with the loss of sleep.
Pheochromocytoma:
Catecholamine secreting tumors in the adrenal medulla can lead to very high levels of circulating catecholamines (both epinephrine and norepinephrine). This leads to α-adrenoceptor mediated systemic vasoconstriction and β-adrenoceptor mediated cardiac stimulation, both of which contribute to significant elevations in arterial pressure. Despite the elevation in arterial pressure, tachycardia occurs because of the direct effects of the catecholamines on the heart and vasculature. Excessive β-adrenoceptor stimulation in the heart often leads to arrhythmias. The pheochromocytoma is diagnosed by measuring plasma or urine catecholamine levels and their metabolites (vanillylmandelic acid and metanephrine).
Preeclampsia:
This is a condition that sometimes develops during the third trimester of pregnancy that causes hypertension, sometimes with fluid retention and proteinuria due to increased blood volume and tachycardia. The former increases cardiac output by the Frank-Starling mechanism.
Arch of the aorta:
Obstruction of the aorta at this point reduces distal arterial pressures and elevates arterial pressures in the head and arms. The reduced systemic arterial pressure activates the renin-angiotensin-aldosterone system, which leads to an increase in blood volume. This further increases arterial pressures in the upper body and may largely offset the reduction in lower body arterial pressures. This condition is readily diagnosed by comparing arterial pressures measured in the arms and legs. Normally, these pressures are very similar, but with coarctation, arterial pressures in the arms can be much greater than arterial pressures measured in the legs. Because this is a chronic condition, the baroreceptors are desensitized and upper body arterial pressures remain elevated because of the increased cardiac output to these parts of the body.
Aortic coarctation:
Coarctation (narrowing) of the aorta is a congenital defect that most commonly is found just distal to the left subclavian artery in the arch of the aorta.
Symptoms of Hypertension:
High blood pressure usually causes no symptoms and high blood pressure often is labeled “the silent killer”. People who have high blood pressure typically do not know it until their blood pressure is measured.
Sometimes people with markedly elevated blood pressure may develop:
• Headache
• Dizziness
• Blurred vision
• Nausea and vomiting, and
• Chest pain and shortness of breath.
People often do not seek medical care until they have symptoms arising from the organ damage caused by chronic (ongoing, long-term) high blood pressure. The following types of organ damage are commonly seen in chronic high blood pressure:
• Heart attack.
• Heart failure.
• Stroke or transient ischemic attack (TIA).
• Kidney failure.
• Eye damage with progressive vision loss.
• Peripheral arterial disease causing leg pain with walking (claudication).
• Outpouchings of the aorta, called Aneurysms
About 1% of people with high blood pressure do not seek medical care until the high blood pressure is very severe, a condition known as malignant hypertension.
• In malignant hypertension, the diastolic blood pressure (the lower number) often exceeds 140 mm Hg.
• Malignant hypertension may be associated with headache, lightheadedness, nausea, vomiting, and stroke-like symptoms.
• Malignant hypertension requires emergency intervention and lowering of blood pressure to prevent brain hemorrhage or stroke.
It is of extreme importance to realize that high blood pressure can be unrecognized for years, causing no symptoms but causing progressive damage to the heart, other organs, and blood vessels.
Diagnosis of Hypertension:
High blood pressure is diagnosed based on the results of a blood pressure test. The test yields two numbers: systolic and diastolic. Blood pressure values are often written as systolic pressure/diastolic pressure; for example, 120/80. The unit of measurement for blood pressure is millimeters of mercury (mmHg).
Blood Pressure Categories in Adults:
The National Heart, Lung, and Blood Institute divide blood pressure levels into several categories. Below are the values that define each of these categories in adults.
Normal:
Systolic pressure, less than 120 mmHg, and Diastolic pressure, less than 80 mmHg.
Prehypertension:
Systolic pressure, 120-139 mmHg or Diastolic pressure, 80-89 mmHg.
Stage 1 high blood pressure:
Systolic pressure, 140-159 mmHg or Diastolic pressure, 90-99 mmHg.
Stage 2 high blood pressure:
Systolic pressure, 160 mmHg and above or Diastolic pressure, 100 mmHg and above. When systolic and diastolic pressures fall into different categories, the higher one is used. For example, a blood pressure reading of 165/85 is considered stage 2 high blood pressure.
Isolated systolic hypertension:
It refers to high blood pressure in which only the systolic number is high. It occurs in about two-thirds of people over age 60 who have high blood pressure. This condition should be taken as seriously as high blood pressure in which both values are elevated because it can cause just as much harm if left untreated.
Diagnosis in Children and Teens:
Blood pressure is measured the same way in children and teens as it is in adults. However, the younger and smaller the child, the lower the values normally are. To diagnose high blood pressure, the blood pressure values for a particular child or teen are compared to average blood pressure readings for young people of the same age, gender, and height.
The following points are also taken into consideration in diagnosis:
1. Medical and family history
2. Physical examination
3. Ophthalmoscopy
4. Chest-X-ray
5. Electrocardiograph
6. Blood and urine tests
Treatment of Hypertension:
There is no cure for primary hypertension but blood pressure can almost always be lowered with the correct treatment. The goal of treatment is to lower blood pressure to levels that will prevent heart disease and other complications of hypertension.
In secondary hypertension, the disease that is responsible for the hypertension is treated in addition to hypertension itself. Successful treatment of the underlying disorder may cure secondary hypertension.
Antihypertensive medicines fall into several classes of drugs (see table)
Prevention of Hypertension:
Having high blood pressure can be prevented by eating healthily, maintaining a healthy weight, taking regular exercise, drinking alcohol in moderation and not smoking, reducing salt intake, managing stress.
Table: Antihypertensive drugs
| Classification | Mechanism of action | Examples |
| Central acting agents | These prevent the brain from signaling the nervous system to increase heart rate and narrow blood vessels. | Clonidine and methyldopa |
| Calcium Channel Blockers | These vasodilate the blood vessels and slow heart rate by blocking calcium channel | Amlodipine, Felodipine, Nicardipine, Nifedipine, Diltiazem verapamil |
| Drugs acts on the RAA system | Vasodilatation of blood vessels. Decreases release of renin. Antagonize the angiotensin II receptor. | Captopril, Enalapril Aliskiren Losartan, Telmisartan |
| Anti-adrenergic drugs | Vasodilatation of blood vessels Reduces conduction of nerve impulses to blood vessels. | Atenolol, Metoprolol Doxazosin, Phentolamine Carvedilol, Labetalol |
| Aldosterone Receptor Antagonists | Block aldosterone that can lead to salt and fluid retention, which can contribute to high blood pressure. | Eplerenone, Spironolactone |
| Diuretics | Eliminate sodium and water, reducing blood volume. | Ethacrynic acid, Furosemide hydrochlorothiazide and chlorothiazide. |
Make sure you also check our other amazing Article on : Atherosclerosis