Introduction of Leprosy:
Table of Contents
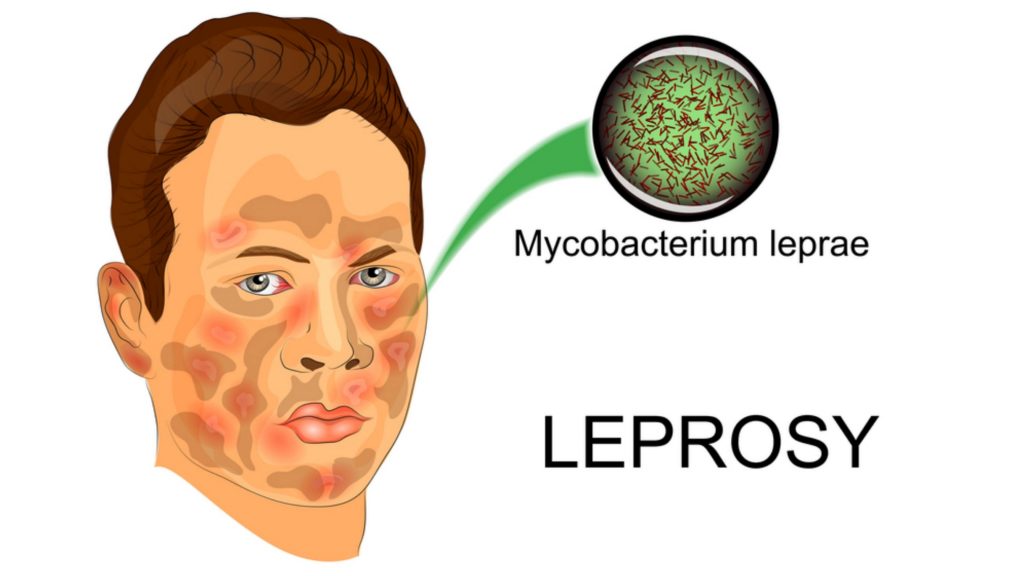
Leprosy (also known as Hansen’s disease) is an infection caused by slow-growing bacteria called Mycobacterium leprae. It is a slowly developing (from six months to 40 years), progressive disease that damages the skin and nervous system. It results in skin lesions and deformities, most often affecting the cooler places on the body (for example, eyes, nose, earlobes, hands, feet, and testicles). The skin lesions and deformities can be very disfiguring and are the reason that infected individuals historically were considered outcasts in many cultures. Although human-to-human transmission is the primary source of infection, three other species can carry and (rarely) transfer M. leprae to humans: chimpanzees, mangabey monkeys, and nine-banded armadillos. The disease is termed a chronic granulomatous disease, similar to tuberculosis because it produces inflammatory nodules (granulomas) in the skin and nerves over time.
The disease has been known to man since time immemorial. DNA taken from the shrouded remains of a man discovered in a tomb next to the old city of Jerusalem shows him to be the earliest human proven to have suffered from leprosy. The remains were dated by radiocarbon methods to 1–50 A.D. The disease probably originated in Egypt and other Middle Eastern countries as early as 2400 BCE. An apparent lack of knowledge about its treatment facilitated its spread throughout the world. Mycobacterium leprae, the causative agent of leprosy, was discovered by G. H. Armauer Hansen in Norway in 1873, making it the first bacterium to be identified as causing disease in humans. Over the past 20 years, the WHO implementation of MDT has rendered leprosy a less prevalent infection in 90% of its endemic countries with less than one case per 10,000 populations. Though, it continues to be a public health problem in countries like Brazil, Congo, Madagascar, Mozambique, Nepal, and Tanzania.
Leprotic patients can be classified into three groups, each with slightly different signs and symptoms:
Paucibacillary (PB), or tuberculoid, Hansen’s disease: It is characterized by one or a few hypopigmented or hyperpigmented skin macules that exhibit loss of sensation (anesthesia) due to infection of the peripheral nerves supplying the region. The body’s immune response may also result in swelling of the peripheral nerves; these enlarged nerves may be palpated under the skin, and may or may not be tender to the touch. The nerves most often found to have swelling are:
- Great auricular nerve,
- Ulnar nerve above the elbow and dorsal cutaneous branches at the wrist,
- Median nerve at the wrist (in the carpal tunnel),
- Radial nerve (superficial at the wrist),
- Common peroneal nerve (also femoral cutaneous and lateral popliteal nerves where they wind around the neck of the fibula),
- Posterior tibial nerve, posterior to the medial malleolus,
- Sural nerve.
Multibacillary (MB), or lepromatous, Hansen’s disease: It is characterized by generalized or diffuse involvement of the skin, a thickening of the peripheral nerves under microscopic examination, and has the potential to involve other organs, the eyes, nose, testes, and bone. The nodular form of this condition is the most advanced form of the disease. Ulcerated nodules contain large numbers of M. leprae acid-fast bacilli packed in macrophages that appear as large foamy cells. MB form of Hansen’s disease is associated with:
- Multiple, symmetrically-distributed skin lesions that might not exhibit loss of sensation,
- Nodules and Plaques,
- Thickened dermis,
- Frequent involvement of the nasal mucosa resulting in nasal congestion and epistaxis.
Borderline, or dimorphous, Hansen’s disease: It is the most common form. When compared to tuberculoid or lepromatous forms, it is of intermediate severity. The skin lesions seem to be of the tuberculoid type, but are more numerous, and may be found anywhere on the body. Peripheral nerves are affected as well, with ensuing weakness and anesthesia.
Pathogenesis of Leprosy:
The onset of leprosy is insidious. It affects nerves, skin, and eyes. It may also affect mucosa (mouth, nose, and pharynx), testes, kidneys, voluntary/smooth muscles, reticuloendothelial system, and vascular endothelium.
Bacilli enter the body usually through the respiratory system. It has low pathogenicity, only a small proportion of infected people develop signs of the disease. Though infected, the majority of the population does not develop the disease. After entering the body, bacilli migrate towards the neural tissue and enter the Schwann cells. Bacteria can also be found in, macrophages, muscle cells, and endothelial cells of blood vessels.
After entering the Schwann cells or macrophage; the fate of the bacterium depends on the resistance of the infected individual towards the infecting organism. Bacilli start multiplying slowly (about 12-14 days for one bacterium to divide into two) within the cells, get liberated from the destroyed cells, and enter other unaffected cells. Till this stage, the person remains free from signs and symptoms of leprosy.
As the bacilli multiply, bacterial load increases in the body, and infection is recognized by the immunological system. Lymphocytes and histiocytes (macrophages) invade the infected tissue. At this stage, the clinical manifestation may appear as the involvement of nerves with impairment of sensation and/or skin patch. If it is not diagnosed and treated in the early stages, further progress of the disease is determined by the strength of the patient’s immune response. Specific and effective cell-mediated immunity (CMI) protects a person against leprosy. When specific CMI is effective in eliminating/ controlling the infection in the body, lesions heal spontaneously or it produces paucibacillary (PB) type of leprosy. If CMI is deficient; the disease spreads uncontrolled and produces multi-bacillary (MB) leprosy with multiple system involvement. Sometimes, the immune response is abruptly altered, either following treatment (MDT) or due to improvement of immunological status, which results in the inflammation of the skin or/and nerves and even others tissue, called as leprosy reaction (types 1 and 2).
Epidemiology:
M. leprae is a fastidious, acid-fast, intracellular pathogen. In 2008, there were approximately 250,000 new cases reported, predominantly in India, Brazil, and Indonesia. Humans were previously thought to be the only important reservoirs of the bacteria, but it is now appreciated that leprosy, or Hansen’s disease, may also be acquired from environmental sources. Leprosy is likely transmitted by aerosol droplets taken up through nasal or another upper airway mucosa, where it has been detected by PCR techniques. A large number of organisms have been found in the nasal secretions of lepromatous leprosy patients.
Symptoms of Leprosy:
Symptoms mainly affect the skin, nerves, and mucous membranes (the soft, moist areas just inside the body’s openings). The disease can cause skin symptoms such as:
- Discolored patches of skin, usually flat, that may be numb and look faded (lighter than the skin around).
- Growths (nodules) on the skin.
- Thick, stiff, or dry skin.
- Painless ulcers on the soles of feet.
- Painless swelling or lumps on the face or earlobes.
- Loss of eyebrows or eyelashes.
Symptoms caused by damage to the nerves are:
- Numbness of affected areas of the skin.
- Muscle weakness or paralysis (especially in the hands and feet).
- Enlarged nerves (especially those around the elbow and knee and in the sides of the neck).
- Eye problems that may lead to blindness (when facial nerves are affected).
Symptoms caused by the disease in the mucous membranes are:
- A stuffy nose and nose bleeds.
Since Hansen’s disease affects the nerves, loss of feeling or sensation can occur. When loss of sensation occurs, injuries such as burns may go unnoticed. Because you may not feel the pain that can warn you of harm to your body. Take extra caution to ensure the affected parts of your body are not injured. If left untreated, the signs of advanced leprosy can include:
- Paralysis and crippling of hands and feet,
- Shortening of toes and fingers due to reabsorption,
- Chronic non-healing ulcers on the bottoms of the feet,
- Blindness,
- Loss of eyebrows,
- Nose disfigurement,
- Painful or tender nerves,
- Redness and pain around the affected area,
- Burning sensation in the skin.
Diagnosis of Leprosy:
The majority of cases of leprosy are diagnosed by clinical findings, especially since most current cases are diagnosed in areas that have limited or no laboratory equipment available. Hypopigmented patches of skin or reddish skin patches with loss of sensation thickened peripheral nerves, or both clinical findings together often comprise the clinical diagnosis. Skin smears or biopsy material that show acid-fast bacilli with the Ziehl-Neelsen stain or the Fite stain (biopsy) can diagnose multibacillary leprosy, or if bacteria are absent, diagnose Paucibacillary leprosy. Other tests can be done, but most of these are done by specialized labs and may help a clinician to place the patient in the more detailed Ridley-Jopling classification and are not routinely done (lepromin test, phenolic glycolipid-1 test, PCR, lymphocyte migration inhibition test, or LMIT). Other tests such as CBC test, liver function tests, creatinine test, or a nerve biopsy may be done to help determine if other organ systems have been affected.
Treatment of Leprosy:
- Paucibacillary leprosy is treated with two antibiotics, dapsone, and rifampicin, while multibacillary leprosy is treated with the same drugs, in addition with another antibiotic, clofazimine. Usually, antibiotics are given for at least six to 12 months or more to cure the disease.
- Multibacillary leprosy can be kept from advancing and living. M. leprae can be essentially eliminated from the person by antibiotics, but the damage that occurred before the administration of antibiotics is usually not reversible. Recently, the WHO suggested that single-dose treatment of patients with only one skin lesion with rifampicin, minocycline (Minocin), or ofloxacin (Floxin) is effective.
- Steroid medications have been used to minimize pain and acute inflammation with leprosy.
Complications:
Without treatment, leprosy can permanently damage your skin, nerves, arms, legs, feet, and eyes. Complications of leprosy can include:
- Blindness or glaucoma.
- Disfiguration of the face (including permanent swelling, bumps, and lumps).
- Erectile dysfunction and infertility in men.
- Kidney failure.
- Muscle weakness that leads to claw-like hands or an inability to flex the feet.
- Permanent damage to the inside of the nose, which can lead to nose bleeds and a chronic, stuffy nose.
- Permanent damage to the nerves outside the brain and spinal cord, including those in the arms, legs, and feet.
Prevention of Leprosy:
The prevention of leprosy ultimately lies in the early diagnosis and treatment of those individuals suspected or diagnosed as having leprosy, thereby preventing further transmission of the disease to others.
- Public education and community awareness are crucial to encourage individuals with leprosy and their families to undergo evaluation and treatment with MDT.
- Household contacts of patients with leprosy should be monitored closely for the development of leprosy signs and symptoms.
- A study demonstrated that prophylaxis with a single dose of rifampicin was 57% effective in preventing leprosy for the first two years in individuals who have close contact with newly diagnosed patients with leprosy.
- There is currently no widely used standard for using medications for the prevention of leprosy.
- Currently, there is no single commercial vaccine that confers complete immunity against leprosy in all individuals.
- Several vaccines, including the BCG vaccine, provide variable levels of protection against leprosy in certain populations.
Make sure you also check our other amazing Article on : Typhoid Fever