Definition of Adaptation
Table of Contents
Adaptation refers to the process by which a system seeks to restore or maintain homeostasis. The adaptive mechanism may also be referred to as compensatory mechanisms, homeostatic mechanisms, control, and regulatory mechanism. Although adaptation may be physiological, psychological, behavioural, in system terminology adaptive mechanisms are examples of feedback to the system and may be represented by either negative or positive feedback loops.
Negative Feedback Loops:
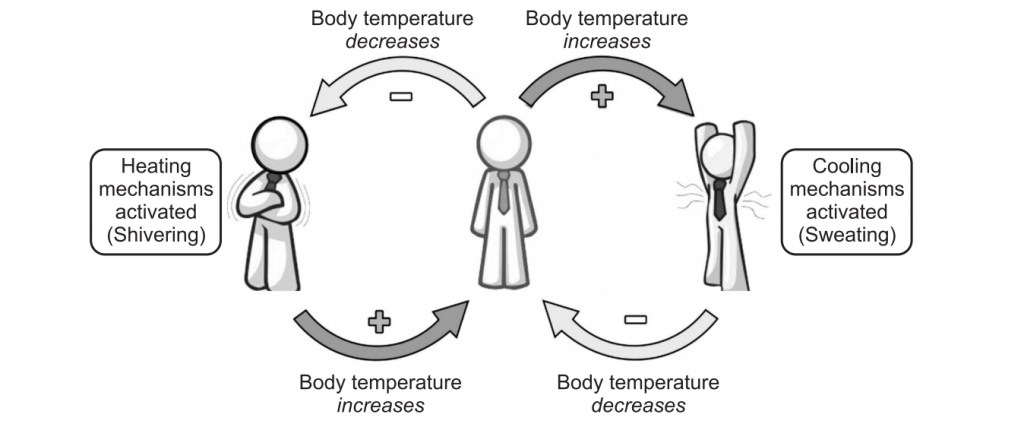
Nearly, all physiologic adaptive responses are negative feedback loops. These processes act to restore homeostasis by inducing changes in the opposite direction of a force perturbing the system.
For example, if injury with haemorrhage causes a decrease in blood pressure, sensors in blood vessels activate neural responses that cause an increase in cardiac pumping and constriction of blood vessels. These changes cause an increase in blood pressure a change that negates the original disruption, completing the feedback loop and restoring the steady-state. Other examples of Homeostasis are temperature control is vital to the maintenance of homeostasis within the body. Heat is sensed by thermoregulators in both, the skin and the hypothalamus. The internal temperature is sensed by the hypothalamus, and external temperature is sensed by the skin. When the external temperature outside is too cold, messages are sent from the many thermoreceptors located within the skin to the cerebellum leading to the hypothalamus.
The role of the cerebellum is to make the individual aware of feeling cold, which may cause voluntary behavioural changes such as putting on more layers of clothing or a coat.
Once the message is received by the hypothalamus, a series of reactions follow. The first of which is by the hypothalamus, which secretes thyroid releasing hormone (TRH). This hormone’s target is the anterior lobe of the pituitary gland. When the TRH reaches its target, it releases Thyroid Stimulating Hormone (TSH) which enters the bloodstream and stimulates the thyroid gland to produce thyroxin. The role of thyroxin is to increase cellular metabolism to generate heat. This hormone also inhibits vasoconstriction, the process in which blood is diverted from the skin to conserve heat by keeping it deep within the body. Sweating is also reduced to keep the surface of the skin dry, thus preventing heat loss. In addition to all of these processes, the erector pili muscles contract, causing the skin hairs to stand erect. This traps air between the hairs and the skin and creates a layer of insulation, therefore keeping the body warmer. In addition, the phenomenon of shivering is displayed and the bodies’ metabolic rate is increased.
When the body temperature increases, messages are sent in the same way as if the body is cold to the hypothalamus. This causes an increase in the amount of sweating, this is releasing heat via water, and the water on the skin evaporates, cooling the body down. Vasodilatation is also apparent. In this instance, blood is diverted to the skin to lose heat. The erector pili muscles relax, allowing the skin hairs to be lowered, and the bodies’ metabolic rate is reduced. The reactions are different for each of the environmental states as the messages sent for each are different.
Water balance is another very important aspect of homeostasis, which needs to be controlled within narrow limits. The control of water balance is conducted using the following series of events. The osmoreceptors located within the hypothalamus detect the condition of fluid balance within the body. If the fluid balance is too low, then the hypothalamus will act to bring the level back, by keeping more water within the body. If the concentration of water within the body is too high, then the hypothalamus will react to excrete more water from the body. In the event of the hypothalamus sensing a change in fluid balance, messages are sent to the cerebellum, from where a feeling of thirst is produced. This is only when there is not enough water within the body. In addition, the hypothalamus sends a message also to the posterior pituitary gland to induce the secretion of ADH. The action of the ADH in this instance is to increase the permeability of the collecting duct of the kidney and increase the amount of water that is reabsorbed into the body.
Blood glucose is another contributing factor to homeostasis. The blood glucose concentration in the blood is vital to the functioning of cells within the body and is controlled by several internal structures and external influences (food and drink). If too much glucose is present within the blood, then specific receptors located within the pancreas detect this. These receptors then send messages to the cerebellum, feelings of satiety (feeling full) are induced, and therefore the individual’s intake of food is decreased. Messages are also sent to the islets of Langerhans for the production of insulin to commence. Once insulin is produced, it is secreted into the capillary circulation and eventually into the systemic bloodstream. Insulin has many effects, mainly consisting of increasing the intake of glucose by all the cells of the body. This action uses up surplus glucose and brings back a stable equilibrium. The insulin also aids in the conversion of glucose into a substance called glycogen in the liver, thus lowering the level of glucose in the blood and restoring equilibrium.
On the other hand, if there is not enough glucose in the bloodstream, then the very same receptors, which are located in the pancreas, detect the change. Once again, a message is sent to the cerebellum, which brings around feelings of hunger, therefore increases the consumption of food and drink. Messages are also sent to cells in the islets of Langerhans to start the production of glucagon. This glucagon is released by the islets of Langerhans into the capillary circulation. In turn, the systemic bloodstream stimulates the liver to convert stored glycogen into glucose. In addition, the liver is stimulated also to start the conversion of amino acids into glucose, therefore the levels of glucose in the bloodstream rise, and equilibrium is achieved.
Homeostasis is also heavily involved with the control of the respiratory rate. In the norm, individuals are not conscious of their respiration. This is because the act of respiration is involuntary. Respiration is under involuntary control through an area of the brain termed the medulla. Within the medulla is an area known as the breathing centre. The breathing centre is composed of sections, allowing each to tackle an alternate aspect of respiration. Both the dorsal and the lateral areas assist with inspiration and provide stimulation for respiration. In addition, the ventral area increases both the depth and rate of respiration. The centre is linked with the intercostal nerves and the phrenic nerves, leading to the diaphragm. These routes provide a method of communication between the thorax, the respiratory system, and the medulla.
The medulla is chief in maintaining a constant rate of respiration and depth. However, both external and internal stimuli can alter the rate of respiration, making it higher or lower than the norm. The main influence to this is the level of carbon dioxide in the bloodstream. If the concentration of carbon dioxide in the bloodstream increases, then chemoreceptors located within both aortic and carotid bodies become aroused. Medulla receives sensory impulses from chemoreceptors, and integrated impulses are sent to the intercostal muscles and the diaphragm through phrenic and intercostal nerves. This causes them to contract and relax more quickly and therefore increase the breathing rate, introduce more oxygen to the bloodstream and bring back the equilibrium of both oxygen and carbon dioxide levels in the bloodstream. This process is an example of negative feedback.
As for the control of the breathing rate, the medulla also controls the heart rate. The set process for the regulation of the heart rate is rather complex and is as follows. As an individual exercise, special receptors located within the muscles send impulses to the medulla. Once these messages are received, the medulla secretes epinephrine and norepinephrine. The combination of these two chemicals proceeds through pathways within the nervous system until they reach the Sinoatrial node, located within the myocardium. It acts like a pacemaker, controlling its electrical activity. These chemicals arouse the Sino-atrial node, making it produce more electrical energy, thus making the heart rate increase.
On the other hand, when exercise is ceased, the muscles send additional impulses to the medulla which respond by secreting the hormone acetylcholine. This hormone decreases the heart rate by slowing down the electrical impulses from the Sino-atrial node and therefore, decreases the heart rate. In addition, the medulla can also recognize other factors which cause an increase in heart rate. These include emotional stress. In this instance, the medulla also takes information from the thalamus, which informs the medulla of the stressor. This is with the addition of information received from the nervous system. The combination of the two would enable the best response possible to be triggered. Homeostatic processes are controlled by negative feedback and hence these systems occur more commonly within the body.
Positive Feedback Loops:
The response to disruptive forces is in the same direction as the force; thus tending to increase the instability of the system. Positive feedback loops are almost always maladaptive or harmful and are often termed vicious cycles, downward spirals, or decompensation states.
These states can lead to death if not interrupted by treatment. In advanced shock, for example, the increased rate and pumping force of the heart eventually increase the demand of the heart muscle for oxygenated blood. The gap between oxygen supply and demand widens, and cardiac failure results. Positive feedback systems generally control infrequent conditions such as ovulation, childbirth, and blood clotting. Two positive feedback mechanisms control the release of oxytocin:
Uterine contractions during childbirth:
When contractions start, oxytocin is released which stimulates more contractions and more oxytocin is released, hence contractions increase in intensity and frequency. Production and release of oxytocin stop after the baby is delivered.
Secretion of breast milk:
The stimulation of a baby sucking its mother’s breast leads to the secretion of oxytocin into the mother’s blood, which leads to milk being available to the baby via the breast. The mother’s production and release of oxytocin cease when the baby stops feeding.
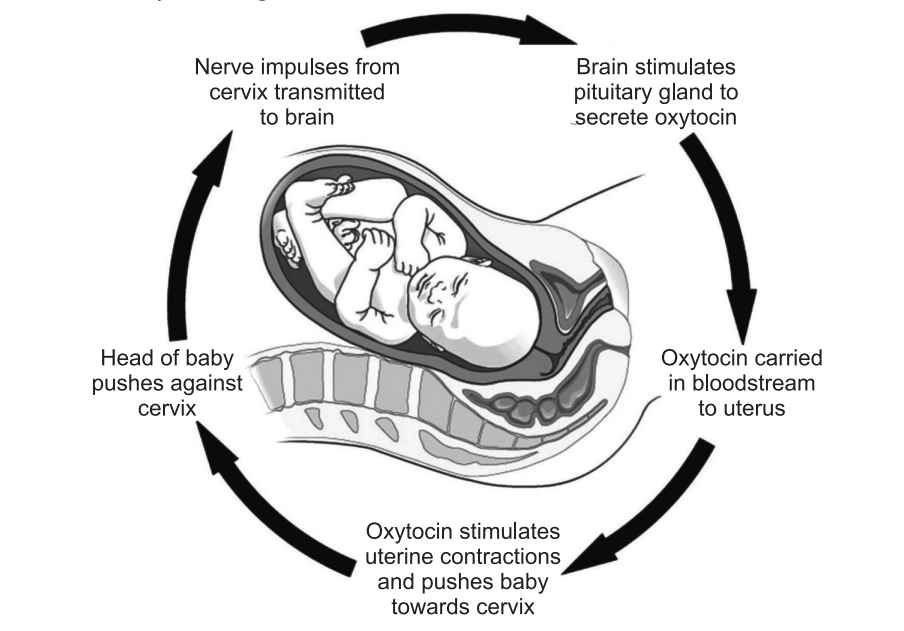
Table: Example for Negative and Positive feedback mechanism
| Negative Feedback mechanism | Positive Feedback mechanism |
| Thermoregulation: If body temperature changes, mechanisms are induced to restore normal levels. | Childbirth: Stretching of uterine walls causes contractions that further stretch the walls (this continues until birth occurs). |
| Blood sugar regulation: Insulin lowers blood glucose when levels are high; glucagon raises blood glucose when levels are low | Lactation: The child feeding stimulates milk production which causes further feeding (continues until the baby stops feeding). |
| Osmoregulation: ADH is secreted to retain water when dehydrated and its release is inhibited when the body is hydrated. | Ovulation: The dominant follicle releases oestrogen which stimulates LH and FSH release to promote further follicular growth. |
| Sex Hormones: The synthesis and release of sex hormones are regulated by a negative feedback mechanism. | Blood clotting: Platelets release clotting factors that cause more platelets to aggregate at the site of injury. |
Make sure you also check our other amazing Article on : Poisons and Antidotes