Introduction of Alzheimer’s disease:
Table of Contents
Alzheimer’s disease (AD) is a progressive, degenerative disorder that attacks the brain’s nerve cells, or neurons especially in the cerebral cortex, resulting in loss of memory, thinking and language skills, and behavioral changes. A degenerative brain disease of unknown cause that is the most common form of dementia or loss of intellectual function, is generally found among people aged 65 and older. A common form of dementia of unknown cause, begin in late middle age, characterized by progressive memory loss and mental deterioration associated with brain damage. A disease marked by the loss of cognitive ability, generally over 10 to 15 years, and associated with the development of abnormal tissues and protein deposits in the cerebral cortex. Alzheimer’s disease is a condition in which nerve cells in the brain die, making it difficult for the brain’s signals to be transmitted properly. Alzheimer’s symptoms may be hard to distinguish early on. A person with Alzheimer’s disease has problems with memory, judgment, and thinking, which makes it hard for the person to work or take part in day-to-day life. The death of the nerve cells occurs gradually over years.
Causes of Alzheimer’s disease:
Like all types of dementia, Alzheimer’s disease is a neurodegenerative disease that results from a combination of genetic, lifestyle, and environmental factors that affect progressive brain cell death over a course of time.
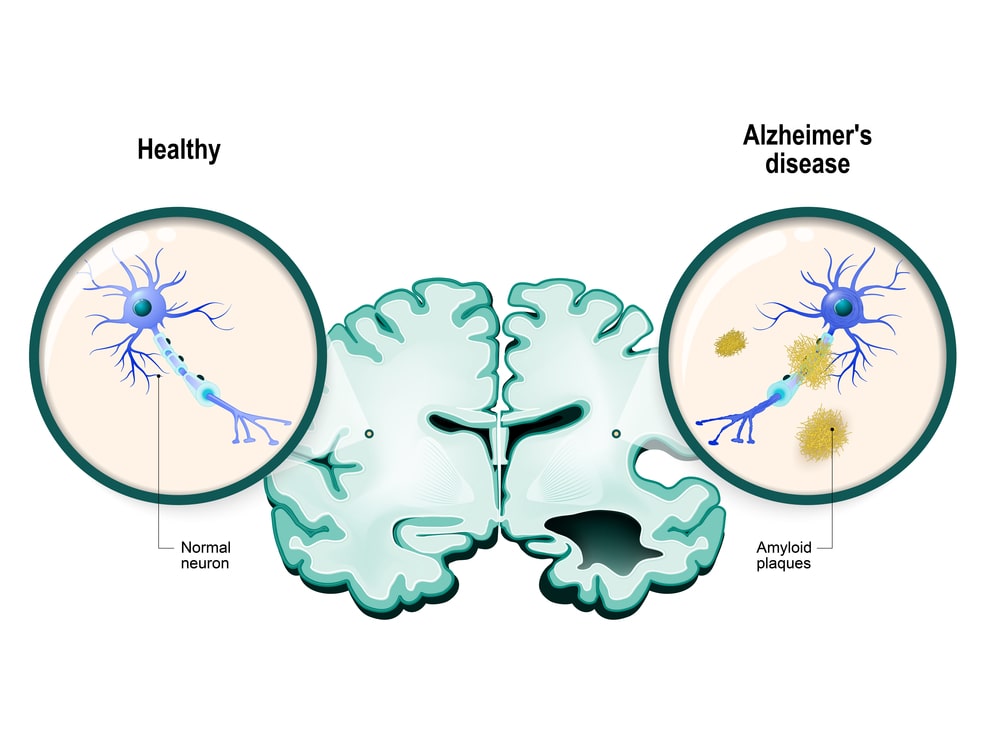
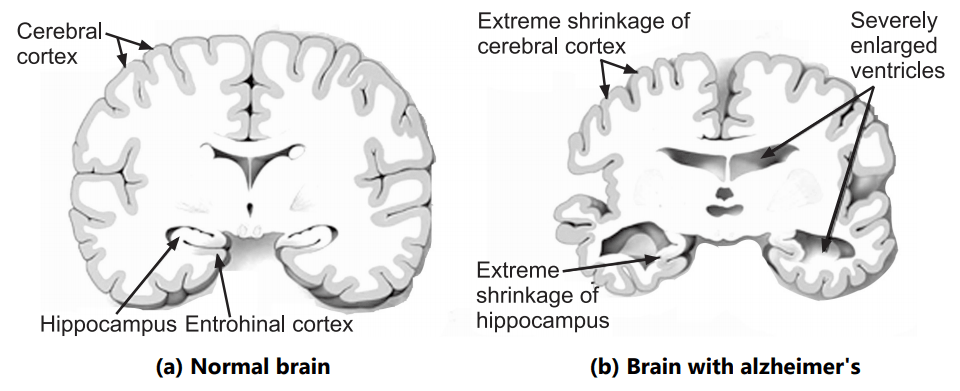
Although the causes of Alzheimer’s are not yet fully understood, its effect on the brain is clear. Alzheimer’s disease damages and kills brain cells. A brain affected by Alzheimer’s disease has many fewer cells and many fewer connections among surviving cells than does a healthy brain. As more and more brain cells die, Alzheimer’s leads to significant brain shrinkage.
Plaques: These clumps of a protein called β-amyloid may damage and destroy brain cells in several ways, including interfering with cell-to-cell communication. Although the ultimate cause of brain-cell death in Alzheimer’s is not known, the collection of β-amyloid on the outside of brain cells is a prime suspect.
Tangles: Brain cells depend on an internal support and transport system to carry nutrients and other essential materials throughout their long extensions. This system requires the normal structure and functioning of a protein called tau.
Loss of nerve cell connections: The tangles and plaques cause neurons to lose their connection to one another and die off.
As the neurons die, brain tissue shrinks (atrophies).
In Alzheimer’s, threads of tau protein twist into abnormal tangles inside brain cells, leading to failure of the transport system. This failure is also strongly implicated in the decline and death of brain cells.
Types of Alzheimer’s disease:
Early-onset AD: Symptoms appear before age 60. This type is much less common than late-onset. However, it tends to get worse quickly. The early-onset disease can run in families. Several genes have been identified.
Late-onset AD: This is the most common type. It occurs in people after age 60 and older. It may run in some families, but the role of genes is less clear.
Symptoms of Alzheimer’s disease:
In most people with Alzheimer’s, the disease progresses slowly, usually over several years. Dementia symptoms include difficulty with many areas of mental function, including Emotional behavior or personality.
Common symptoms of Alzheimer’s disease include:
Impaired memory and thinking: The person has difficulty remembering things or learning new information. In the later stages of the disease, long-term memory loss occurs, the person cannot remember personal information, such as place of birth or occupation, or names of close family members. Forgetting details about current events and forgetting events of own life history.
Disorientation and confusion: People with Alzheimer’s disease may get lost when out on their own and may not be able to remember where they are or how they got there. They may not recognize previously familiar places and situations. They also may not recognize familiar faces or know what time of the day it is, or even what year it is.
Misplacing items: The person forgets where they put items used every day, such as glasses, a hearing aid, keys, etc. The person may also put things in strange places, such as leaving their glasses in the refrigerator.
Abstract thinking: Difficulty performing tasks that take some thought, but used to come easily, such as balancing a checkbook, playing complex games (such as a bridge), and learning new information or routines.
Trouble performing familiar tasks: Difficulty in performing basic tasks, such as preparing meals, choosing the proper clothing, grooming, and driving. Planning for normal day-to-day tasks is also impaired.
Hallucinations, arguments, striking out, and violent behavior: The person becomes unusually angry, irritable, restless, or quiet. At times, people with Alzheimer’s disease can become confused, paranoid, or fearful.
Poor or decreased judgment: People with Alzheimer’s disease may leave the house on a cold day without a coat or shoes or could go to the store wearing pajamas.
Inability to follow directions: The person has difficulty understanding simple commands or directions. The person may get lost easily and begin to wander.
Problems with language and communication: The person cannot recall words, names, and objects (very familiar ones, like a pen), or understand the meaning of common words.
Impaired visual and spatial skills: The person loses spatial abilities (the ability to judge shapes and sizes and the relationship of objects in space) and cannot arrange items in a certain order or recognize shapes.
Loss of motivation or initiative. The person may become very passive and require prompting to become involved and interact with others.
Loss of normal sleep patterns. The person may sleep during the day and be wide awake at night.
Risk Factors of Alzheimer’s disease:
Increasing age is the greatest known risk factor for Alzheimer’s. Alzheimer’s is not a part of normal aging, but the risk increases greatly after age 65. Nearly half of those older than age 85 have Alzheimer’s.
Family history and genetics: The risk of developing Alzheimer’s appears to be somewhat higher if a first-degree relative (parent or sibling) has the disease. Scientists have identified rare changes (mutations) in three genes that virtually guarantee a person who inherits them will develop Alzheimer’s. But these mutations account for less than 5 % of Alzheimer’s disease.
Sex: Women may be more likely than are men to develop Alzheimer’s disease. Mild cognitive impairment has an increased risk.
Past head trauma: People who have had severe head trauma or repeated head trauma appear to have a greater risk of Alzheimer’s disease.
Lifestyle and heart health: Some evidence suggests that the same factors that put at risk of heart disease also may increase the chance to develop Alzheimer’s. Examples include Lack of exercise, Smoking, High blood pressure, High blood cholesterol, Elevated homocysteine levels, poorly controlled diabetes, and a diet lacking in fruits and vegetables.
Diagnosis:
There is no specific test that confirms Alzheimer’s disease. Alzheimer’s disease can be diagnosed with complete accuracy only after death when a microscopic examination of the brain reveals the characteristic plaques and tangles. To help distinguish Alzheimer’s disease from other causes of memory loss, doctors now typically rely on the following types of tests. A skilled health care provider can often diagnose Alzheimer’s disease with the following steps:
Complete physical exam: It includes a neurological exam, medical history, and symptoms which include, reflexes, muscle tone, and strength, ability to get up from a chair and walk across the room, sense of sight and hearing, coordination, and balance.
A mental status examination: A brief mental status test to assess memory and other thinking skills.
A diagnosis of Alzheimer’s disease is made when certain symptoms are present, and by making sure other causes of dementia are not present.
Tests may be done to rule out other possible causes of dementia, including:
- Anemia,
- Brain tumor,
- Chronic infection,
- Intoxication from medication,
- Severe depression,
- Stroke,
- Thyroid disease,
- Vitamin deficiency.
Brain imaging: Images of the brain are now used chiefly to pinpoint visible abnormalities related to conditions other than Alzheimer’s disease such as strokes, trauma, or tumors, that may cause cognitive change.
Brain-imaging technologies include:
Computed tomography (CT) or magnetic resonance imaging (MRI) of the brain may be done to look for other causes of dementia, such as a brain tumor or stroke.
In the early stages of dementia, brain image scans may be normal. In later stages, an MRI may show a decrease in the size of different areas of the brain.
While the scans do not confirm the diagnosis of Alzheimer’s disease, they do exclude other causes of dementia (such as stroke and tumor).
Alzheimer’s disease can be diagnosed with complete accuracy only after death when a microscopic examination of the brain reveals the characteristic plaques and tangles.
The following changes are more common in the brain tissue of people with Alzheimer’s disease:
“Neurofibrillary tangles” (twisted fragments of protein within nerve cells that clog up the cell).
“Neuritic plaques” (abnormal clusters of dead and dying nerve cells, other brain cells, and protein).
“Senile plaques” (areas where products of dying nerve cells have accumulated around protein).
Treatment of Alzheimer’s disease:
Although there is no cure, Alzheimer’s medications can temporarily slow the worsening of symptoms and improve the quality of life for those with Alzheimer’s and their caregivers. The U.S. Food and Drug Administration (FDA) has approved five medications (listed below) to treat the symptoms of Alzheimer’s disease.
Exercise: Regular exercise has known benefits for heart health and may also help prevent cognitive decline. Exercise may also help improve mood.
Nutrition: People with Alzheimer’s may forget to eat, lose interest in preparing meals or not eat a healthy combination of foods. They may also forget to drink enough water, leading to dehydration and constipation.
Prevention:
Although there is no proven way to prevent Alzheimer’s disease, there are some practices that may be worth incorporating into daily routine, particularly with a family history of dementia.
Consume a low-fat diet, eat coldwater fish (like tuna, salmon, and mackerel) rich in ω-3 fatty acids, at least 2 to 3 times per week, reduce intake of linoleic acid found in margarine, butter, and dairy products, increase antioxidants like carotenoids, vitamin E and vitamin C by eating plenty of darkly colored fruits and vegetables, maintain normal blood pressure and stay mentally and socially active throughout life.
Table: The U.S. Food and Drug Administration (FDA) approved medications for Alzheimer’s disease
| Sr. No. | Drug name | Brand name | Approved For | FDA Approved |
| 1 | Donepezil | Aricept | All stages | 1996 |
| 2 | Galantamine | Razadyne | Mild to moderate | 2001 |
| 3 | Memantine | Namenda | Moderate to severe | 2003 |
| 4 | Rivastigmine | Exelon | All stages | 2000 |
| 5 | Donepezil and memantine | Namzaric | Moderate to severe | 2014 |
Make sure you also check our other amazing Article on : Schizophrenia