DEFINITION
Table of Contents
Hypertension is defined as bizarre raise in diastolic and/or systolic pressure.
CLASSIFICATION OF HYPERTENSION
| Classification | Systolic (mmHg) | Diastolic (mmHg) |
| Normal | < 120 | < 80 |
| Pre-hypertension | 120 – 139 | 80 – 89 |
| Stage 1 | 140 – 159 | 90 – 99 |
| Stage 2 | > 160 | > 100 |
Prevalence
Women 55 years of age are more prone to hypertension than men. Blood pressure levels increase with age and it (persistently elevated BP levels) is very common in the elderly.
ETIOLOGY
- In most patients, hypertension results from an unknown pathophysiologic etiology (essential or primary hypertension). This form of hypertension cannot be cured, but it can be controlled.
- A small percentage of patients have a specific cause of their hypertension (secondary hypertension).
Many potential secondary causes are either concurrent medical conditions or are endogenously induced.
If the cause can be identified, hypertension in these patients has the potential to be cured.
Essential Hypertension:
- More than 90% of individuals with hypertension have essential hypertension.
- Numerous mechanisms have been identified that may contribute to the pathogenesis of this form of hypertension, so identifying the exact underlying abnormality is not possible.
- Genetic factors may play an important role in the development of essential hypertension.
Secondary Hypertension:
- Fewer than 10% of patients have secondary hypertension where either a comorbid disease or drug is responsible for elevated BP.
- In most of these cases, renal dysfunction resulting from severe chronic kidney disease or renovascular disease is the most common secondary cause.
- Certain drugs, either directly or indirectly, can cause hypertension or exacerbate hypertension by increasing BP.
Diseases: Chronic kidney disease, Obstructive sleep apnea, Parathyroid disease, Pheochromocytoma, Thyroid disease.
Prescription drugs: Adrenal steroids, Amphetamines/anorexiants, Decongestants, Nonsteroidal anti-inflammatory drugs.
Food substances: Sodium, Ethanol, Licorice.
ANTIHYPERTENSIVE DRUG CLASSES
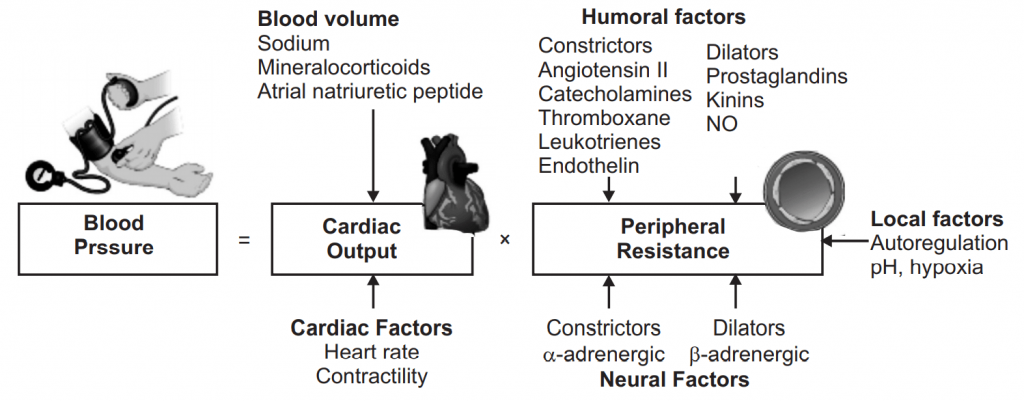
Antihypertensive drugs are organized around a clinical indication − the need to treat a disease − rather than a receptor type. The drugs covered in this unit have a variety of mechanisms of action including diuresis, sympathoplegia, vasodilation, and antagonism of angiotensin, and many agents are available in most categories.
Note: Antihypertensive drugs have then never been more important. Along with diet and exercise, they remain one of the most effective methods to reduce high blood pressure.
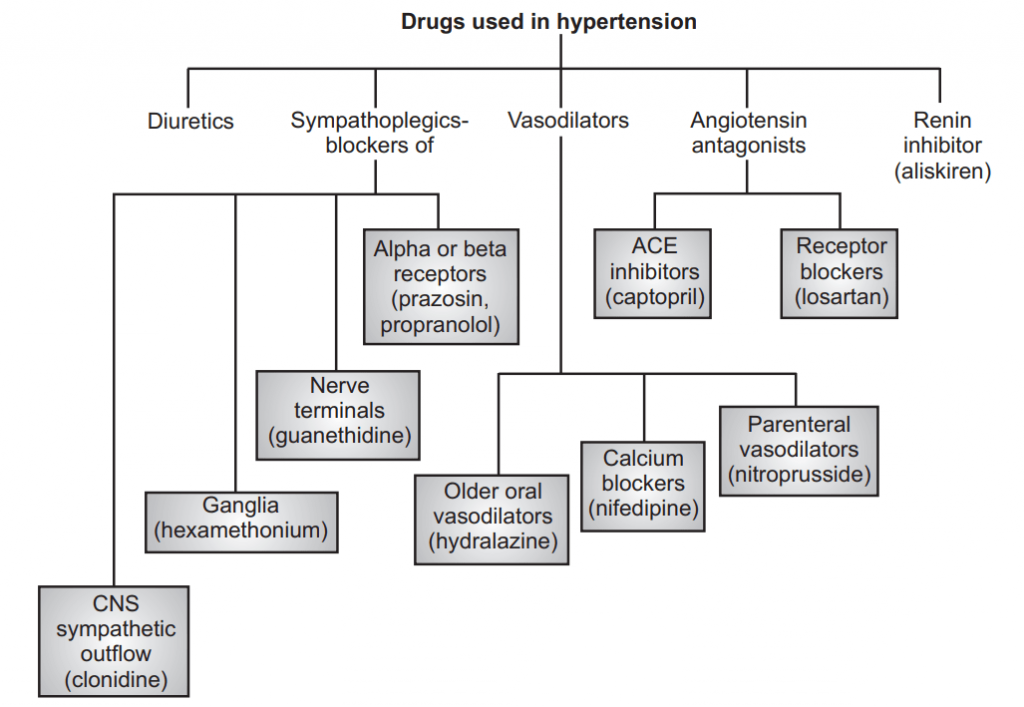
Antihypertensive drug classes are as follows:
- ACE inhibitors
- Angiotensin II receptor antagonists
- Diuretics
- Calcium channel blockers
- β-blockers
- α-blockers
- α2-blockers
- Renin-inhibitors
- Vasodilators
For each drug class, we offer examples, their mechanism of actions (MOA), side effects and drug interaction profiles, and any other relevant clinical features.
1. ACE Inhibitors (Angiotensin-Converting Enzyme Inhibitors (ACEIs))
Example: Ramipril, Lisinopril, Perindopril.
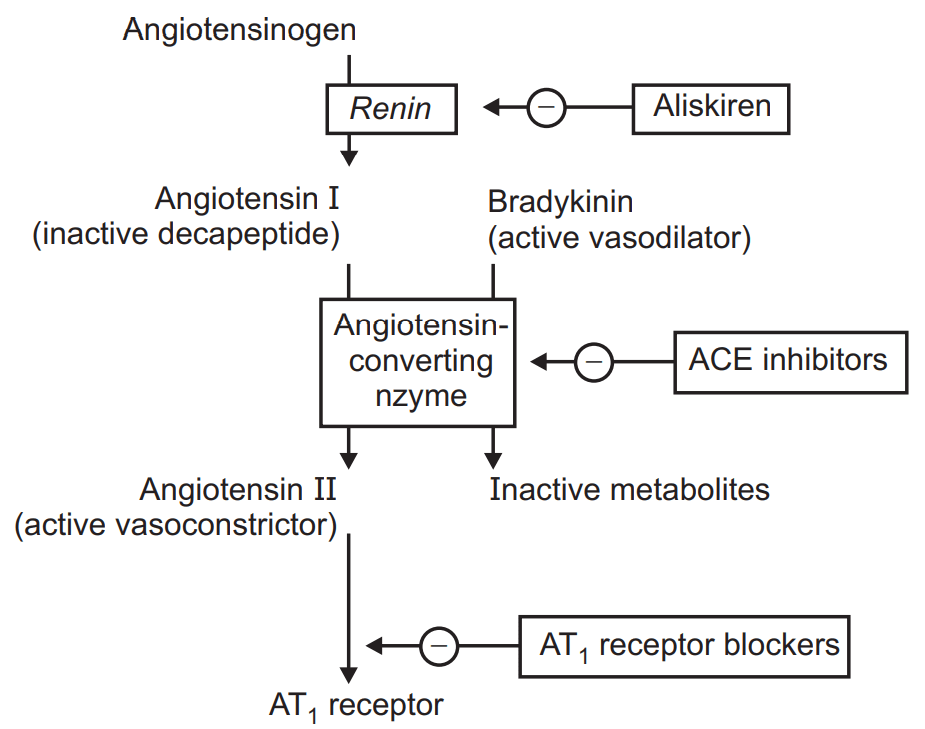
MOA: Angiotensin-converting enzyme inhibitors (ACEIs) are those drugs that are frequently used for the treatment of cardiovascular disorders including hypertension and heart failure. This group of drugs diminishes blood pressure and oxygen demand by dilating blood vessels. These drugs principally inhibit an angiotensin-converting enzyme which is an integral part of RAAS (Renin-angiotensin-aldosterone system). The detailed model of action is described in the following diagram.
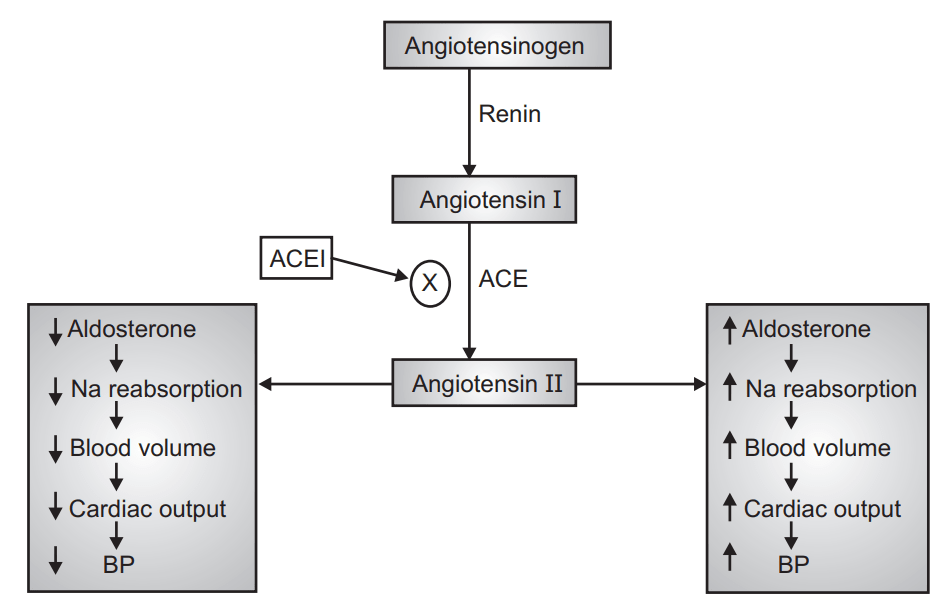
Side effects:
- Hypotension-first dose hypotension is prevalent with ACE inhibitors.
- Persistent dry cough due to pulmonary kinin accumulation.
- Hyperkalemia-ACE inhibitors promote potassium retention.
- Other effects- fatigue, nausea, dizziness, headache.
2. Angiotensin II Receptor Antagonists
Angiotensin II receptor antagonists are also known as ARBs or angiotensin receptor blockers. They are sometimes used in place of ACE inhibitors particularly where the persistent dry cough has become unbearable for the patient.
Examples: Candesartan, lrbesartan, Losartan, Telmisartan.
MoA:
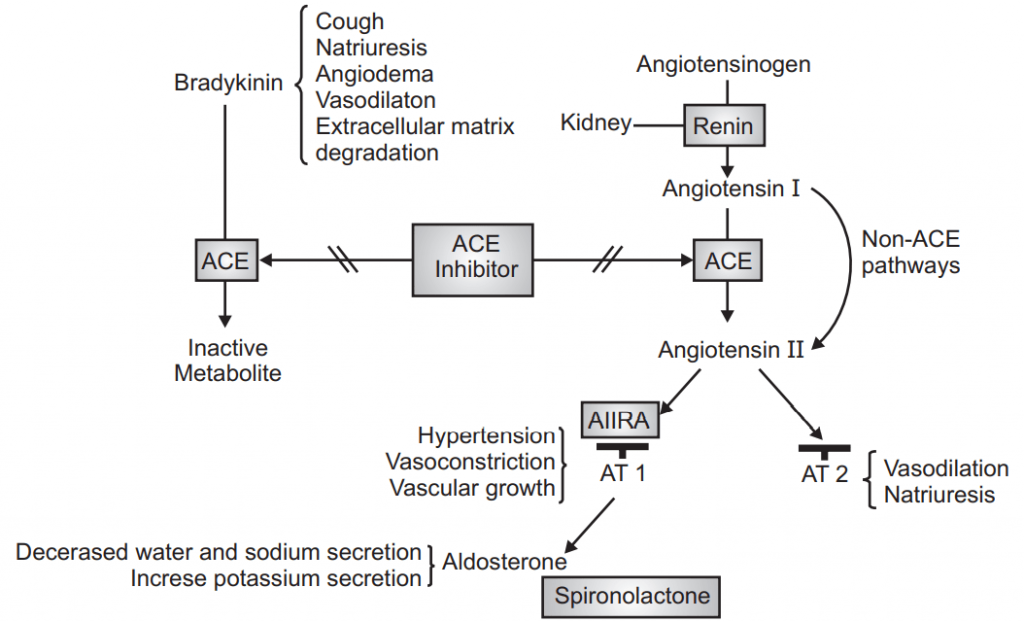
Side effects: Hypotension, Hyperkalemia
Renal failure (as with ACE inhibitors):
- Cough-though is less likely than with ACE inhibitors.
- Due to the risk of hyperkalemia, other potassium-elevating drugs should not be prescribed.
- This includes potassium supplements, potassium-sparing diuretics.
- As with ACE inhibitors, taking ARBs with NSAIDs increases the risk of renal failure.
3. Diuretics
Diuretics are drugs that promote dieresis or water loss. There are many different diuretic classes, too many to review in detail here. However, we have examined many of the major diuretic classes elsewhere.
Diuretic drug classes:
- Loop diuretics-furosemide, bumetanide.
- Thiazide and thiazide – like diuretics – bendroflumethiazide, hydrochlorothiazide, indapamide, metolazone.
- Potassium-sparing diuretics- amiloride, spironolactone.
- The purpose of diuretics is to eliminate excess sodium and water from the body. Some diuretic classes also eliminate potassium, increasing the risk of hypokalemia.
- Other drugs though, such as amiloride and spironolactone, retain potassium ions[1]increasing the risk of hyperkalemia. However, diuretic combinations are invariably used to balance and offset these risks.
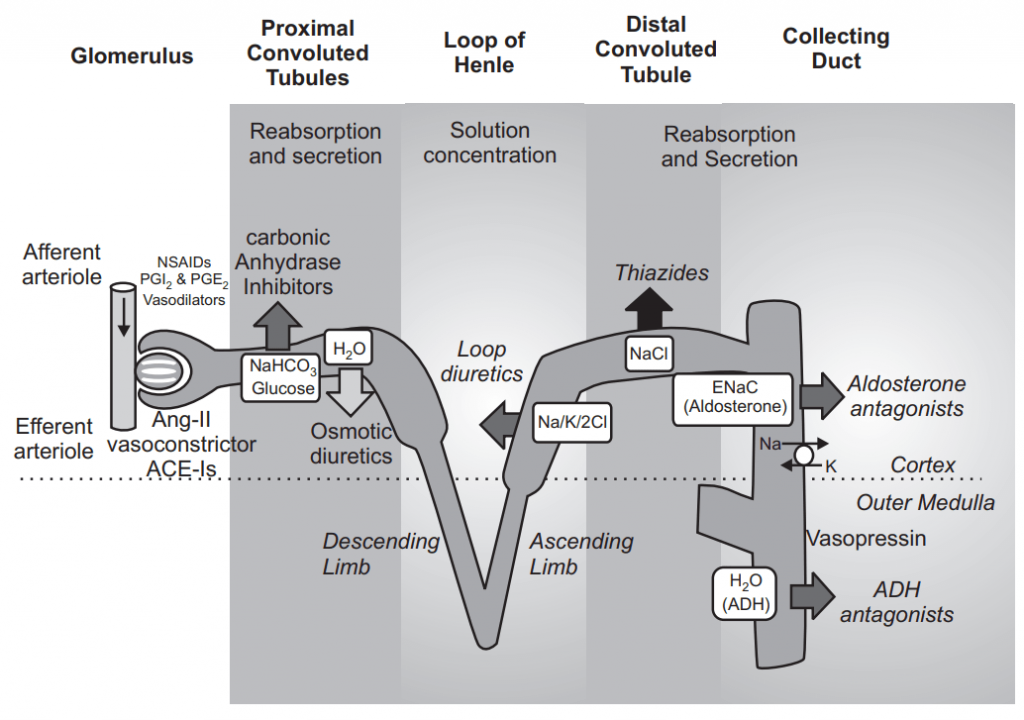
Diuretics act at different points along the nephron:
For example:
- Loop diuretics act at the thick ascending limb.
- Thiazide diuretics act at the distal convoluted tubule.
- Potassium-sparing diuretics act at the cortical collecting duct.
- Osmotic diuretics, such as mannitol, act at the proximal tubule.
- Carbonic anhydrase inhibitors, such as acetazolamide, also act at the proximal tubule.
Side effects: In general terms, the broadside effects associated with diuretics include:
- Loop diuretics: Hypovolemia, hypokalemia, metabolic alkalosis, hyperuricemia.
- Thiazides: Associated with the side effects listed for loop diuretics, plus hypercalcemia and hyponatremia.
- Hyperkalemia: Amiloride, triamterene, spironolactone.
4. Calcium Channel Blockers (CCB)
- Not all calcium channel blockers are used for their antihypertensive effects.
Examples:
- Amlodipine, Nifedipine, Diltiazem, Verapamil.
- Amlodipine and nifedipine may be used for hypertension whereas diltiazem and verapamil are predominantly used to control heart rate/ arrhythmias.
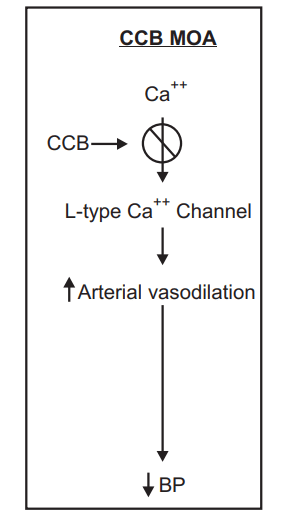
MoA: Calcium channel blockers reduce calcium entry into vascular and cardiac cells. This reduces intracellular calcium concentration which, in turn, causes relaxation on vasodilation in atrial smooth muscle. Calcium channel blockers also reduce myocardial contractility in the heart.
Side effects: Because diltiazem and verapamil (the non-dihydropyridine CCBs) are used as class III anti-arrhythmic drugs, the side effects profile below focuses on amlodipine and nifedipine.
Flushing, Headache, Ankle swelling, palpitations, Light-headedness.
5. β-blockers
β-blockers are not just used in the treatment of hypertension (though not generally given as initial therapy), they are also used in the treatment of ischemic heart disease, chronic heart failure, atrial fibrillation, and supraventricular tachycardia.
Examples: Metoprolol, Bisoprolol, Labetalol, Nebivolol.
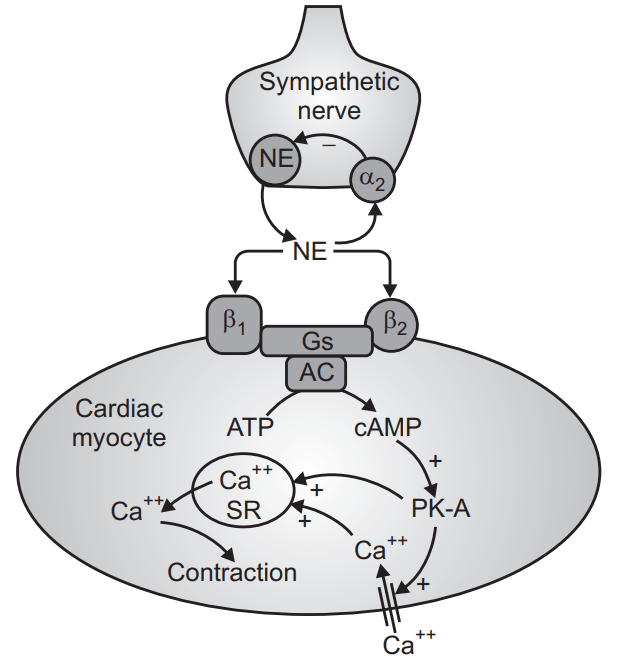
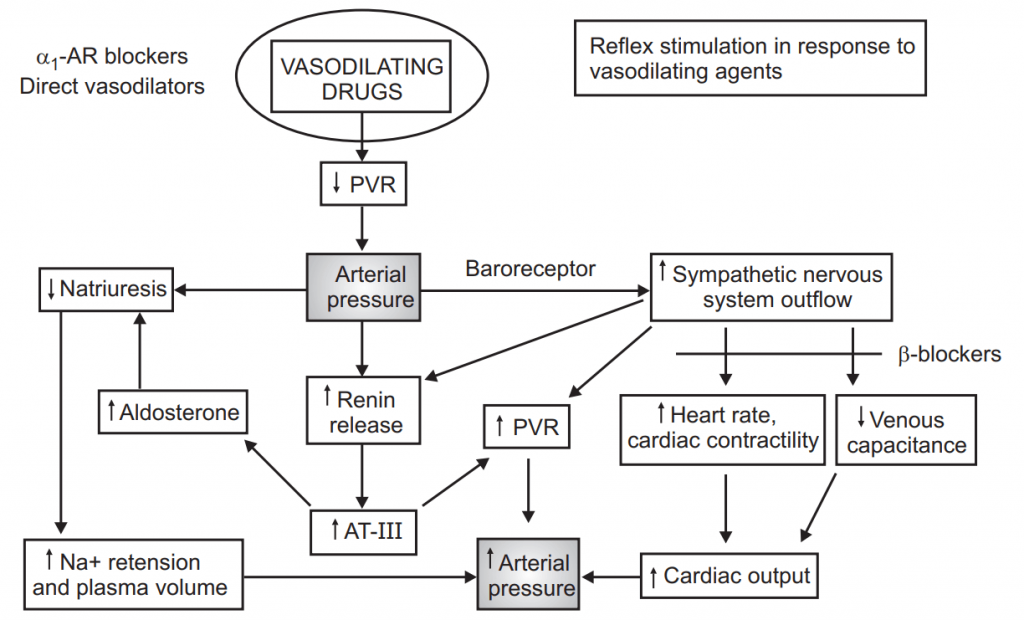
MoA: β-blockers act through a variety of means for hypertension they act to reduce renin secretion from the kidney-an effect ordinarily mediated by β-1 receptors. Recall that β-1 receptors are located mainly in the heart, whereas β-2 receptors are mainly located in the smooth muscle of blood vessels and the airways.
Side effects: Fatigue, Cold extremities, Headache, Nausea.
6. α-blockers
α-blockers may be used to treat hypertension in resistant cases where other drugs –such as ACE inhibitors, calcium channel blockers, and thiazide diuretics-have proven ineffective.
Examples: Alfuzosin, Tamsulosin, Doxazosin.
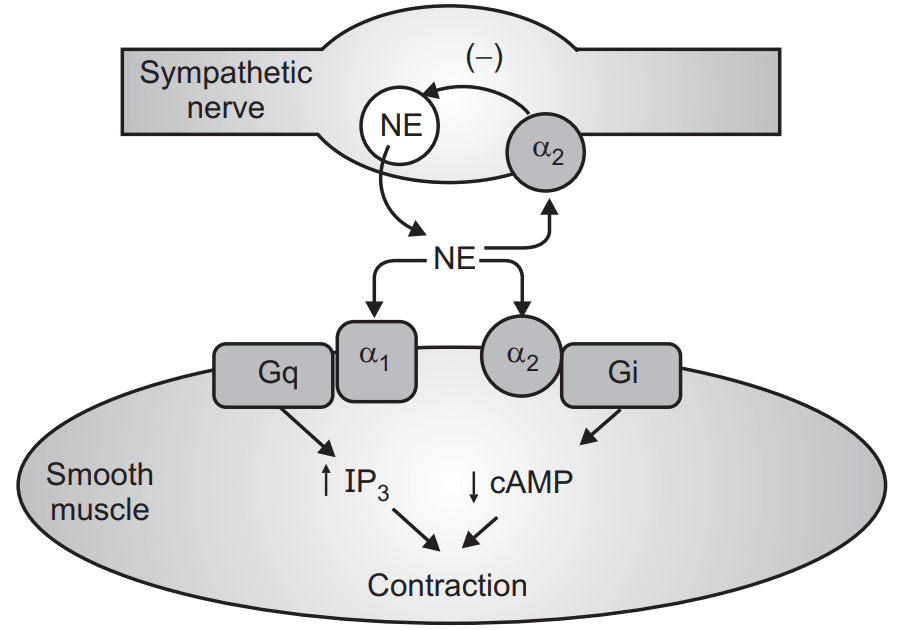
MoA: α-1 receptors are predominantly found in smooth muscle, such as blood vessels or the urinary tract stimulation produces concentration and inhibition causes relaxation α blockers are highly selective for α-1 receptor, causing vasodilation and a reduction in blood pressure.
Side effects: Postural hypotension, Dizziness, Faintness.
These three effects are more pronounced after the first dose.
7. α-2 Agonists
As with the α-2 agonists are rarely used they are typically only used when all other conventional options have been exhausted, when used they are usually taken alongside diuretics.
Examples: Clonidine, Methyldopa, Moxonidine
MoA: More specifically, α-2 agonists are classified as centrally-acting α-2 agonists, these receptors are activated in the brain which, once activated, open peripheral blood vessels around the body, reducing blood pressure.
Side effects: Sedation, dry nasal mucosa, Dry mouth, Rebound hypertension, Postural hypotension, Headache, Fatigue.
8. Renin Inhibitors
Renin is a protein and enzyme secreted by the kidneys.
It works by cleaving angiotensinogen (hepatic-produced) into angiotensin I. ACE then converts angiotensin-I into angiotensin-II and, in turn, angiotensin-II causes increased secretion of aldosterone-increasing blood pressure. Renin-inhibitors are then, an effective way to block the effects of angiotensin-II and reduce blood pressure.
Examples: Aliskiren
MoA:
Side effects: Angioedema, Hyperkalemia, Hypotension, Diarrhea, Headache, Dizziness. Aliskiren should not be taken alongside an angiotensin-receptor blocker or ACE inhibitor in diabetic patients due to an increased risk of stroke, hyperkalemia, and kidney complications.
Due to the above risk and side effect profile, many clinicians regard aliskiren as more harmful than beneficial.
9. Vasodilator
Sodium Nitroprusside: Sodium nitroprusside has been used in cases of hypertensive emergency. It is administered via intravenous route and for this reason, has a rapid onset of effects.
Sodium nitroprusside deploys nitric oxide for its antihypertensive effect. Nitric oxide works to reduce total peripheral resistance and venous return. This reduces both preload and afterload.
Side effects associated with sodium nitroprusside include Hypotension, Methemoglobinemia, Cyanide poisoning, Bradyarrhythmia, Palpitation, Tachyarrhythmia, Confusion, Dizziness, Renal azotemia.
Hydralazine: Hydralazine is used to treat hypertension, though it is more often used to treat high blood pressure, gestational hypertension. Like sodium nitroprusside, it may also be used in a hypertensive emergency.
VASODILATORS:
DIRECT
Side effects: Headache, Tachycardia, Palpitations, Hypotension, Aching/ swelling joints, Flushing.
It works as a direct-acting smooth muscle relaxant, working as a vasodilator in resistance arterioles-decreasing total peripheral resistance and lowering blood pressure.
Make sure you also check our other amazing Article on : Congestive Heart Failure