Introduction of Stroke:
Table of Contents
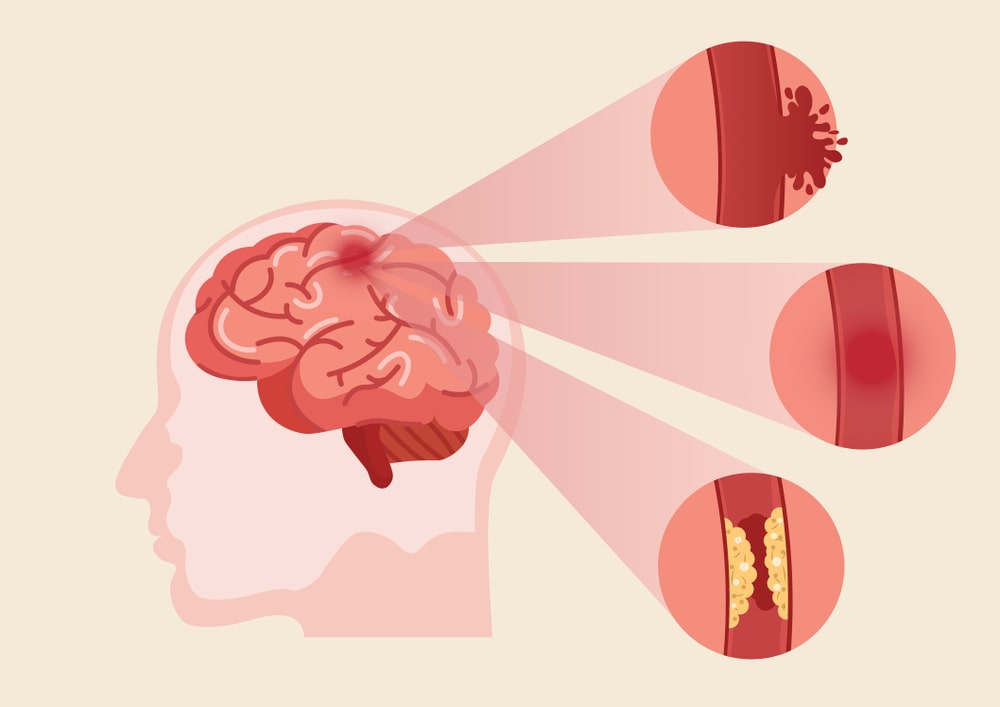
A stroke is a “brain attack”. It occurs when blood flow to an area of the brain is cut off. When this happens, brain cells are deprived of oxygen and begin to die. When brain cells die during a stroke, abilities controlled by that area of the brain such as memory and muscle control are lost. Stroke is also known as cerebrovascular accident (CVA). The effect of stroke depends on where the stroke occurs in the brain and how much the brain is damaged. For example, someone who had a small stroke may only have minor problems such as temporary weakness of an arm or leg. People who have larger strokes may be permanently paralyzed on one side of their body or lose their ability to speak. Some people recover completely from strokes, but more than 2/3 of survivors will have some type of disability.
Types of Stroke:
There are three main kinds of stroke:
- Ischemic strokes,
- Hemorrhagic strokes,
- Transient ischemic attacks (TIAs), also referred to as mini-strokes.
Causes of Stroke:
The different forms of stroke have different specific causes.
Causes of Ischemic Stroke: Ischemic stroke is the most common form, accounting for around 85 % of strokes. This type of stroke is caused by blockages or narrowing of the arteries that provide blood to the brain, resulting in ischemia – severely reduced blood flow that damages brain cells. These blockages are often caused by blood clots, which can form either in the arteries within the brain, or in other blood vessels in the body before being swept through the bloodstream and into narrower arteries within the brain. Fatty deposits within the arteries called plaque can cause clots that result in ischemia.
Causes of Hemorrhagic Stroke: Hemorrhagic strokes are caused by arteries in the brain either leaking blood or bursting open. The leaked blood puts pressure on brain cells and damages them. It also reduces the blood supply reaching the brain tissue after the hemorrhage point. Blood vessels can burst and spill blood within the brain or near the surface of the brain, sending blood into the space between the brain and the skull. The ruptures can be caused by conditions such as hypertension, trauma, blood-thinning medications, and aneurysms (weaknesses in blood vessel walls). Intracerebral hemorrhage is the most common type of hemorrhagic stroke and occurs when brain tissue is flooded with blood after an artery in the brain bursts. Subarachnoid hemorrhage is the second type of hemorrhagic stroke and is less common. In this type of stroke, bleeding occurs in an artery in the subarachnoid space – the area between the brain and the thin tissues that cover it.
Causes of Transient Ischemic Attack (TIA): TIAs are different from the kinds above because the flow of blood to the brain is only briefly interrupted. TIAs are similar to ischemic strokes. In that, they are often caused by blood clots or other clots. TIAs should be regarded as medical emergencies just like the other kinds of stroke, even if the blockage of the artery and symptoms are temporary. They serve as warning signs for future strokes and indicate that there is a partially blocked artery or clot source in the heart.
Risk Factors:
- Uncontrolled hypertension,
- Diabetes mellitus,
- Smoking,
- Cardiac disease,
- Hyperlipidemia,
- Excessive alcohol intake.
Epidemiology:
Stroke is one of the leading causes of death and disability in India. The estimated adjusted prevalence rate of stroke range, 84-262/100,000 in rural and 334-424/ 100,000 in urban areas. The incidence rate is 119-145/100,000 based on recent population-based studies. There is also a wide variation in the case of fatality rates with the highest being 42% in Kolkata. Stroke units are predominantly available in urban areas that too in private hospitals. Intravenous (IV) and intra-arterial thrombolysis (IA) are commonly used in India.
Pathophysiology of Stroke:
The pathophysiology of stroke is complex and involves numerous processes, including energy failure, loss of cellular ion homeostasis, acidosis, increased intracellular calcium levels, excitotoxicity, free radical-mediated toxicity, generation of arachidonic acid products, cytokine-mediated cytotoxicity, complement activation, disruption of the blood-brain barrier (BBB), activation of glial cells, and infiltration of leukocytes.
Glutamate excitotoxicity: A significant portion of ischemia-induced neuronal damage is mediated by excessive accumulation of excitatory amino acids, leading to a toxic increase in intracellular calcium. Although this is an intrinsic defensive response to protect against ischemia by activating a reaction to severe cell stress, paradoxically, this increase in intracellular calcium activates multiple signaling pathways, which ultimately leads to cell death. In the reduction or termination of cerebral blood flow, energy-dependent cellular pumps fail due to a fall in glucose-dependent ATP generation, resulting in the flow of numerous ionic species into the cell. This results in cellular swelling through osmosis and cellular depolarization. Calcium ions (Ca2+) enter the cell through voltage-dependent and ligand-gated ion channels, resulting in activation of several proteases, kinases, lipases, and endonucleases, triggering the intrinsic apoptotic pathway and thus ending in cell death by Glutamate, which is the major excitatory neurotransmitter in the brain, accumulates in the extracellular space following ischemia, and activates its receptors.
Oxidative stress: The oxidative stress and apoptosis are closely linked phenomena in the pathophysiology of ischemic stroke. Neurons are normally exposed to a baseline level of oxidative stress from both exogenous and endogenous sources, as are all cells in the body. Free radicals like superoxide anion radical, hydroxyl radical, and nitric oxide (NO) produced by mitochondria are involved in stroke-induced brain injury. Free radicals can react with DNA, proteins, and lipids, causing varying degrees of damage and dysfunction.
Oxygen-free radicals can also be generated by activated microglia and infiltrating peripheral leukocytes via the NADPH oxidase system following reperfusion of ischemic tissue. This oxidation causes further tissue damage and is thought to be an important trigger molecule for apoptosis after ischemic stroke.
Lipid peroxidation: Lipid peroxidation plays a prominent role in the pathogenesis of stroke. The mechanism, whereby membrane lipid peroxidation induces neuronal apoptosis, involves the generation of an aldehyde called 4-Hydroxynonenal (4-HNE), which covalently modifies membrane transporters such as the Na+ /K+ ATPase, glucose transporters, and glutamate transporters, thereby impairing their function.
Inflammation and Leucocyte Infiltration: Inflammation in stroke is characterized by the accumulation of leukocytes and activation of resident microglial cells. Inflammatory cells can contribute to stroke pathology through two basic mechanisms. They form aggregates in the venules after reperfusion, or, enter infarcted tissue and exacerbate cell death through the production of free radicals and cytokines. Cell adhesion molecules such as selectins, integrins, and ICAMs permit endothelial-inflammatory cell interactions.
Symptoms of Stroke:
Strokes occur quickly, so symptoms often appear suddenly and without warning. The main symptoms of a stroke are:
Muscular: Difficulty walking, paralysis with weak muscles, problems with coordination, stiff muscles, overactive reflexes, or paralysis of one side of the body.
Whole-body: Balance disorder, fatigue, light-headedness, or vertigo.
Visual: Blurred vision, double vision, sudden vision loss, or temporary loss of vision in one eye.
Speech: Difficulty in speaking, slurred speech, or speech loss.
Sensory: The reduced sensation of touch, even by applying pins and needles.
Facial: Muscle weakness or numbness.
Limbs: Numbness or weakness.
Common: Difficulty in swallowing, headache, inability to understand, mental confusion, or rapid involuntary eye movement.
Facts on Stroke:
- During a stroke, the brain does not receive enough oxygen or nutrients, causing brain cells to die.
- Ischemic strokes are caused by a narrowing or blocking of arteries to the brain.
- Hemorrhagic strokes are caused by blood vessels in and around the brain bursting or leaking.
- Strokes need to be diagnosed and treated as quickly as possible to minimize brain damage.
- Treatment depends on the type of stroke.
- The most effective way to prevent strokes is through maintaining a healthy lifestyle and treating underlying conditions that are risk factors.
Diagnosis:
Several different types of diagnostic tests can be used to determine which type of stroke has occurred:
- Physical examination: It consists of measurement of blood pressure, listens to the carotid arteries in the neck, and examine the blood vessels at the back of the eyes, all to check for indications of clotting.
- Blood tests: A doctor may perform blood tests to find out how quickly the patient’s blood clots. The levels of particular substances (including clotting factors) in the blood, and whether or not the patient has an infection.
- CT scan: A series of X-rays that can show hemorrhages, strokes, tumors, and other conditions within the brain.
- MRI scan: Radio waves and magnets create an image of the brain to detect damaged brain tissue.
- Carotid ultrasound: An ultrasound scan to check the blood flow in the carotid arteries and to see if there is any plaque present.
- Cerebral angiogram: Dyes are injected into the brain’s blood vessels to make them visible under X-ray, to give a detailed view of the brain and neck blood vessels.
- Echocardiogram: A detailed image of the heart is created to check for any sources of clots that could have traveled to the brain to cause a stroke.
Prevention:
- Eating a healthy diet.
- Maintaining a healthy weight.
- Exercise regularly.
- Do not smoke.
- Avoiding alcohol or drink moderately.
- Keeping blood pressure under control.
- Managing diabetes.
- Treating obstructive sleep apnea (if present).
Treatment of Stroke:
Drug Treatment: There is only one Food and Drug Administration (FDA) approved drug treatment for acute ischemic stroke. Tissue plasminogen activator (tPA) is given via intravenous therapy (IV) and works by dissolving the clot and improving blood flow to the part of the brain being deprived of blood flow. tPA should be given within three hours (and up to 4.5 hours in certain eligible patients) of the time symptoms first started.
Mechanical Devices: Some ischemic strokes are treated with small mechanical devices that remove or break up blood clots. If clot-busting drugs are ruled out, another option one of the many FDA-approved mechanical devices. A surgeon inserts a small mechanical device into the blocked artery using a thin tube. Once inside, the tool traps the clot, and either break it up or the surgeon pulls it out of the brain, reopening the blocked blood vessel in the process.
A hemorrhagic stroke (sometimes called a bleed) occurs if an artery in a brain leaks blood or ruptures (breaks open). The first step in treating a hemorrhagic stroke is to find the cause of bleeding in the brain and then control it. Some of the options for treatments include surgical clips or coils inserted in aneurysms (weaknesses in the blood vessel wall), controlling high blood pressure, and surgery to remove the bleeding vessel and blood that has spilled into the brain.
Make sure you also check our other amazing Article on : Parkinson’s Disease