Medication Adherence: Doctors assume that when they give a prescription to a patient, the drug will be taken, as directed. In many of the cases, patients do not follow the instruction regarding prescribed drugs and results in no therapeutic response to given prescribed drugs which indicate poor compliance. Hippocrates warned that patients may ‘often lie about taking their medicines’.
Causes of Medication Non-Adherence
Non-adherences to drug therapy is a very common phenomenon in all patients. There are so many factors that contribute to in-patient non-adherence such as patient views and characters, illness, social issues, service provided. The factors which contribute to non-compliance/non-adherence may come from an external source or patient experience. External factors are those factors that come from outside and that have the potential to impact compliance. All of the factors that contribute to a patient’s experience using prescriptions are known as patient experience.
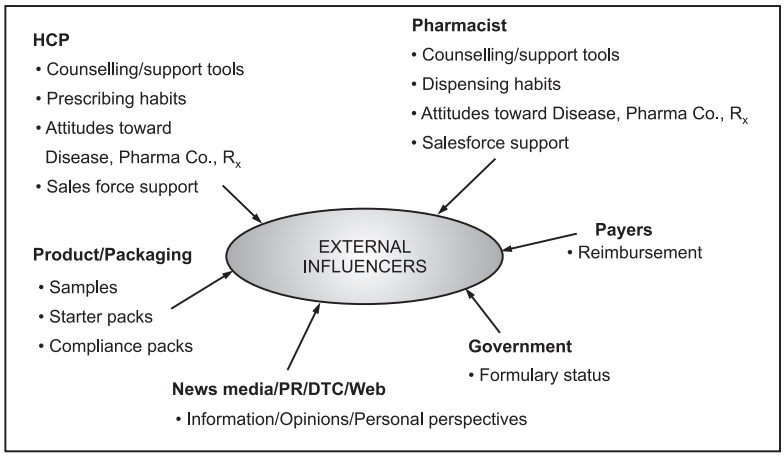
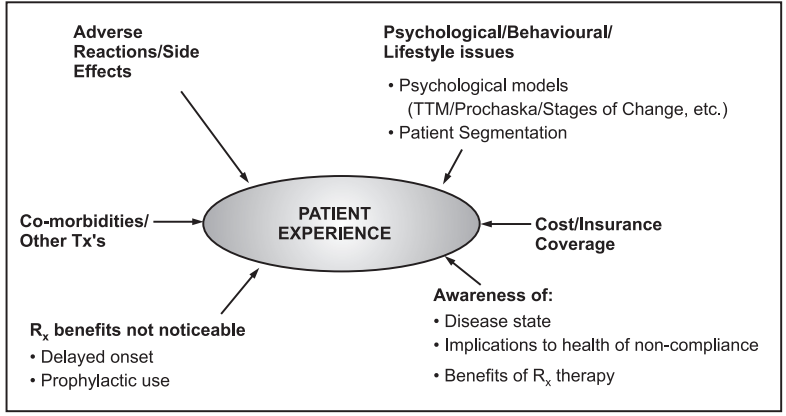
There are various barriers to the effective use of medicines specifically including inadequate knowledge about a drug and its use; poor provider-patient communication; not being influenced for treatment; fear of adverse effects of the prescribed drug; long term and complex drug regimens with varying dosing schedules; cost and access barriers.
Adherence to drug therapy varies with the patient’s age group also. In children, compliance to drug therapy is influenced due to their dependence on a care giver. As per the literature, the compliance report in elderly patients indicates the rates range roughly from 38%-57% with an average rate of less than 45%.
A major reason for non-compliance is higher dis-coordination in patient-physician, which results in decreased patient satisfaction. Several study reports indicate that 40-60% of the patient could not correctly report to the physician while other interviewed report says over 60% of patient get misunderstood the direction regarding prescribed medication.
Non-adherence can also occur in complex drug regimens which could include inappropriate timing of drug administration or administration of several drugs at unusual times during the day. In such cases, a poor therapeutic outcome may occur. At some time, there is variation in the taking of drugs that occurs in terms of omission of dose or delays in the timing of doses.
In most chronic diseases like hypertension, the patient most often becomes non-compliant. The reason for non-compliance is due to the absence of any symptoms even without strict compliance to the therapeutic regimen. From study report, it indicates the higher rates of non-compliance when the patients are symptoms free. The compliance rate dropped considerably when the regimen was taken for a long period.
Another factor that results in patient non-compliance is medications instruction which is difficult to read. Higher rates are observed in low literacy patients. Gender, cultural factors, and personality may affect compliance rates. As per the survey report, there is a higher rate of adherence to the regimen in women than men.
Role of Healthcare Providers to Improve Medication Adherence
The effectiveness of a therapeutic regimen depends upon both the patient adherence and efficacy of the medicine. Thus, healthcare providers, as well as the system, have a great role in improving medication adherence. Improving in a single factor cannot provide a 100% success rate in compliance. There is a need to use a combination of various techniques to improve patient’s adherence to the prescribed therapy. Following are some approaches that can be implemented to improve compliance.
1. Level of Prescribing:
For improving compliance there is a need to introduce two-way approaches during prescribing the medicine. Before prescribing the medicine, a doctor should discuss or ask the patient for a convenient preparation/dosage form and according to the possibility, a doctor should prescribe or change the treatment plan.
2. Communicating with the Patient:
- At the time of prescribing or dispensing of drugs, the health practitioners should explain the key information such as; what, why, when, how, and how long to take medicine.
- The common side effects may result after the use of the regimen and if it is necessary to know to a patient then should be explained by health practitioners.
- To improve patient compliance then provide a medication calendar, medication chart, drug information sheet, special container indicating a time of dose, etc.
- To improve patient compliance, it is necessary to provide behavioral support. Sometimes there is also a need to collaborate with patients to incorporate the medication regimen in their daily schedule particularly when there is a complex therapeutic regimen and in elderly patients.
During Follow-Ups:
For monitoring the patient compliance to medication there should be criteria for the patient follow-up. There are several methods as mentioned earlier can be used to measure patient compliance during follow-up of patients. This should be done by physicians as well as pharmacists.
Compliance may be improved in four ways:
(1) By Ensuring Compliance:
- Doctors and nurses can give a single dose of a drug, for example, gonorrhea can be treated by a single dose of procaine penicillin.
- For the outpatient department, a depot formulation for implantation or intramuscular injection can be given at specified regular intervals, for example, in schizophrenia depot, intramuscular injection of fluphenazine decanoate is given at regular intervals.
- The patient can be supervised while taking the drug by their care-takers, for example; parents can supervise their children while taking a drug, in-hospital visitors can supervise relatives, a nurse can supervise the elderly while taking drugs.
(2) By removing Barrier to Compliance:
There are several barriers to compliance such as the taste of medicine, dosage form, side effects notice, etc. So, some strategies can be used to remove the barrier to increase medicines adherence.
- The sweetness of medicines can be improved by adding flavoring in formulation for children such as the banana flavor of antibiotics.
- For people who have difficulty swallowing tablets, elixirs can be used instead of tablets especially in children and elderly people.
- If the certain formulation causes adverse effects such as diarrhea by ferrous sulfate then formulation must change to slow-release iron formulations. While the effectiveness of such medicines may be less in such cases.
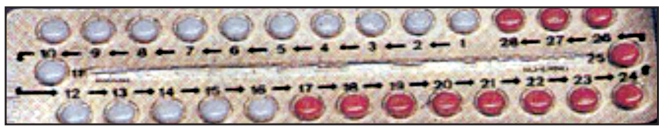
- Use of calendar pack to remind the patient to take their medicines such as blister packs of oral contraceptives or beta-blockers.
(3) By Simplifying Therapeutic Regimens:
Many times, patients avoid or discontinue using drugs due to complex regimens. Doctors can simplify the therapeutic regimen by reducing the number of tablets and frequencies of drug administration. Doctors can prescribe a combination of drugs in a single tablet. Frequent administration of a drug can be avoided by prescribing sustain dosage forms or long-acting drugs. For example: sustain release glibenclamide and metformin in diabetes and morphine for chronic pain. The advantage of such kind of sustain released preparation is minimizing adverse effects.
(4) By Educating the Patient:
In certain conditions (diabetes, tuberculosis, HIV), compliance can be improved by educating the patients about their disease condition and the necessity of medicines for their treatment. Patient education is always to be encouraged if it improves compliance.
A patient can also be helped by providing the leaflets for drug information and instruction to take the medicine particularly for ear drops, pessaries, and suppository.
At each visit patients should bring their tablets with them this allows the doctors to know exactly what drugs the patient is taking. For monitoring the compliance as well as demonstrating the correct method of drug administration patient was asked to have the medicine in front of the physician. This process can help sort out practical aspects of the regimen.
Monitoring of Patients Medication Adherence
There are several methods reported to measure compliance. The method of measuring compliance can be grouped into direct and indirect methods of measurement. Each method has advantages as well as some limitations. But no one considers as a gold standard to measure patient compliance. The simplest way of measuring adherence is from the patient’s self-report.
Adherence to drugs in children can be done by asking questions to care giver. The easy-to-use methods for assessment of drug adherence are questioning the patients, checking patient diaries, and assessment of clinical response. Among these questioning patients regarding compliance indicates misinterpretation and results in overestimating the patient adherence.
Methods of assessing compliance include:
Direct Method:
- Measuring the concentration of the drug in body fluids (Direct method).
- Measuring the pharmacological effect (Direct Method).
Indirect Method:
- Tablet counting
- Patient self-report
- Patient diaries
- Recording devices
- Refilling of Prescription
Measuring patient compliance by using direct methods such as; directly observed therapy, measuring the concentration of drug or its metabolites in a biological fluid, etc. are very most accurate methods but they are very expensive and generally used in research purposes and clinical trials. While in such methods, variation in metabolism can give a false impression of compliance. Differences in bioavailability and renal clearance also influence the quantitative profile of drugs.
Indirect methods for assessing the compliance include patient questionnaires, pill counts, patient self-reports, electronic medication monitors, rates of prescription refills, as well as checking patient diaries.
The reports suggested that patient compliance cannot predict accurately than by chance, thus specific methods should be used for assessing the compliance. Sometimes direct questioning can be asked to a patient regarding adherence to drug therapy.
If the doctor asks the questions tactfully, then the patient is more willing to admit defaulting in adherence.
An example of tactful questions is “Have you managed to take all the tablets?” rather than “Have you missed any tablets?”
Table.1: Methods of Assessing Compliances
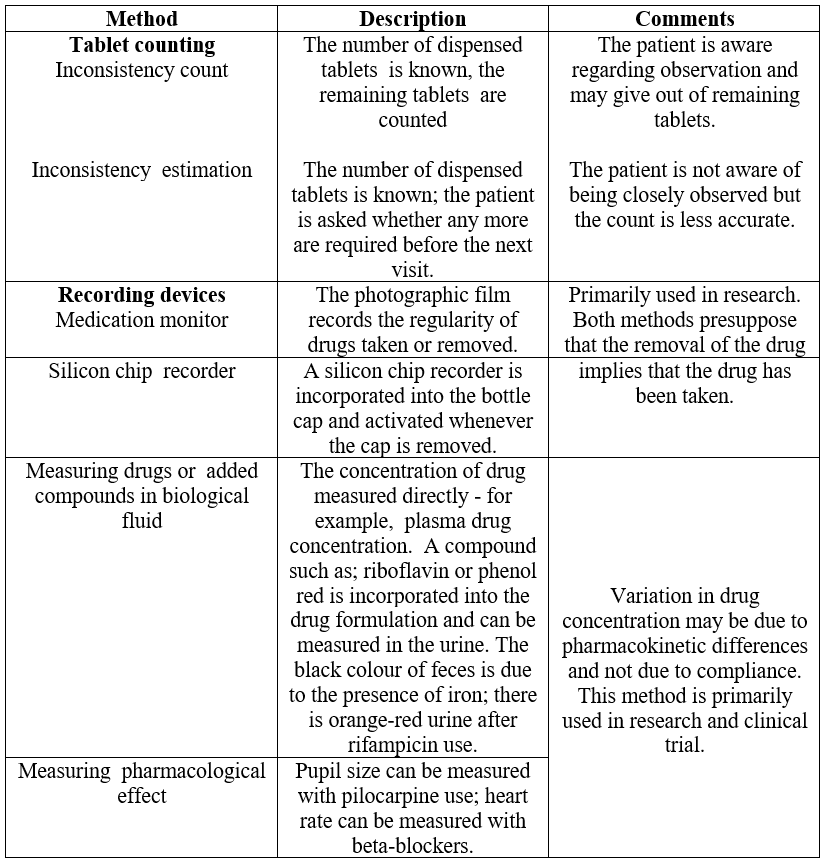
Counting of remaining pills in patient medications bottles or vials is a very common method of assessing compliance. The pill count method is very simple but it has so many disadvantages such as; discarding the remaining pills before a visit to the hospital. Thus, this is not the ideal method to assess compliance. This method does not give information on dose timing and drug holidays.
Rates of refilling prescriptions are a truthful measure of the whole adherence in a closed pharmacy system since refills are measured at several points in that time.
Electronic monitor methods are also giving compliance information. In this method, there is recording and stamping the time of opening bottles, dispensing drops, or activating canister (metered dose inhaler for asthma). The disadvantage of this method is that patients may open the bottle of medicine but are not guaranteed to take medicine. Patients may take the wrong amount of medicine or may take multiple doses.
Checking patient self-report is a common and convenient method for assessing compliance. The report of the patient can be obtained from standard interviews or simple questionnaires regarding the use of drugs. This method is relatively inexpensive. This method provides accurate information even of the unobservable experience and behavior of a patient. For example, patients explain reasons for their non-compliance due to some of the adverse effects of drugs.
Another indirect method for assessment of compliance is checking of patient diaries involves the daily recording by a patient on a drug used. This method provides the assessment of compliance for all drugs and the entire period. While the limitation is the method required more time for the evaluation of the diary as well as entry of large recorded events. The major limitation of this method is in the completion of the diary. Completion of a diary is impossible for those patients who have a problem with literacy, loss of vision, or memory.
Make sure you also check our other amazing Article on : Hospital Formulary
