National Tuberculosis Control Programme: The infectious disease commonly caused by the bacterium Mycobacterium tuberculosis is tuberculosis. TB affects the lungs mainly and causes pulmonary tuberculosis. The other parts of the body, including the intestine, bones and joints, lymph glands, skin, and other body tissues, are also affected by TB.
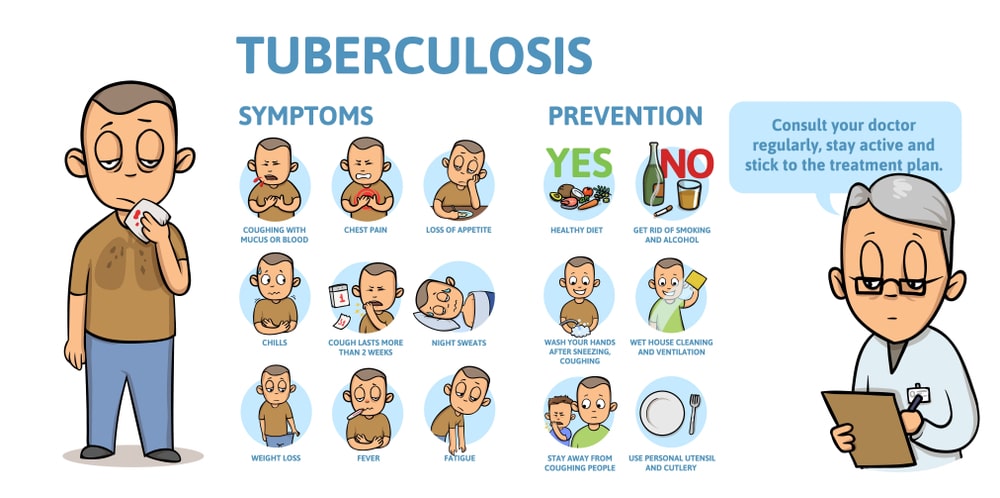
There are no signs in most infections in which the medication is known as latent tuberculosis. A chronic cough with blood-containing sputum, fever, weight loss, and night sweats is the classic sign of active TB.
In people with HIV/AIDS and in those who smoke, active infections occur more frequently. When people who have active TB in their lungs; cough, spit, talk or sneeze, tuberculosis spreads through the air.
Active tuberculosis diagnosis is based on chest x-rays, as well as on microscopic examination and body fluid culture. TB depends on skin tests or blood tests for tuberculin.
More than 10 million cases of active TB occurred in 2016, contributing to 1.3 million deaths. This makes it the number one cause of an infectious disease’s death. In developed countries, more than 95% of deaths occurred, and more than 50% occurred in India, China, Indonesia, Pakistan, and the Philippines. Since 2000, the number of new cases per year has declined.
National Health Programme for Tuberculosis and its Functioning
Table of Contents
In 1962, the National Tuberculosis Programme (NTP) for TB Control in India was initiated. This programme couldn’t offer expected results in India. In 1962, a National Tuberculosis Control Programme was initiated by the Government of India to diagnose as many cases of tuberculosis as possible, provide successful care, set up district tuberculosis centers, expand short-course chemotherapy, and centers for tuberculosis.
improve existing training and demonstration Nationally, there are 390 districts staffed by a team of medical and paramedical professionals with completely equipped DTCS (District Tuberculosis Centers). Many of the other 330 TB clinics are based in big cities, looking after the local population.
Furthermore, 17 tuberculosis training and demonstration centers provide paramedical staff, including general practitioners, with basic training. For TB patients there are a total of around 47,000 beds available nationwide. Most patients are treated at home, so only critical cases are hospitalized or those needing surgical care.
Health education targeting the community and general practitioners is also stressed by the National Tuberculosis Programme. To this end, booklets, pamphlets, radio, TV, and newspaper ads are used. Founded in 1953 in Bangalore, the National Institute of Tuberculosis has been involved in research on epidemiological, sociological, and organizational aspects, along with programme monitoring.
The Revised National Tuberculosis Control Program (RNTCP) started as a pilot project in 1993 and was launched as a national programme in 1997, based on the Directly Observed Care, Short-course (DOTS) approach, but rapid NTCP expansion started in late 1998. In 2006, nationwide coverage was reached.
The Revised National Tuberculosis Control Programme has undertaken early and firm steps towards its stated objective of universal access to early quality diagnosis and quality TB treatment for all TB patients. The revised National Tuberculosis Control Programme is being implemented with decentralized tuberculosis testing facilities through 13,000+ designated microscopy centers and free care throughout the nation through 4 explicitly observed treatment centers.
National Strategic Plan for 2012-2017
The 2012-2017, National Strategic Plan (NSP) was included in the country’s 12th Five Year Plan. “Universal access for quality care and treatment for all TB patients in the nation” with an aim of “reaching the unreached” was the theme of the NSP 2012-2017. The key focus was on the early and full diagnosis of all community-based TB cases, including drug-resistant TB and HIV-associated TB, with greater private sector participation in improving treatment for all patients. Important gains have been made during the National Strategic Plan 2012-2017 period in improving support systems, programme architecture, and implementation of the TB control environment.
National Strategic Plan for 2017-2025 for TB Elimination in India
Building on the progress and learning of the last NSP, the National Strategic Plan 2017 – 2025 encapsulates the bold and imaginative steps needed to eradicate Tuberculosis in India by 2030. It is built in line with other policies and global initiatives in the health sector, such as the 2015 draught national health policy, the End TB Strategy of the World Health Organizations (WHO), and the United Nations (UN) Sustainable Development Goals.
Improving TB Surveillance by Transitioning to Case-Based, Web-Based Recording and Reporting (NIKSHAY)
- This information communication technology application was launched on 15th May 2012, by the National informatics centre and central TB Division.
- The data entry of individual TB cases is being done at the block level data entry operator of NHM.
- The system has been extended to include drug-resistant TB cases, online referral and transfer of patients.
TB Co-Morbidities
- TB and Diabetes: The risk of TB among people with diabetes is 2-3 times higher than among those without diabetes.
- Diabetes can worsen the clinical course of TB, and TB can worsen glycaemic control in people with diabetes.
- TB and Smoking: Smoking increases the risk of TB 2-3 fold, and is associated with poor TB treatment results.
- Smoking prevalence is often high among people with TB, and the prevalence of other smoking-related conditions is high as well.
- High smoking prevalence in the population is an important contributor to high TB Burden.
Objectives of National Tuberculosis Control Programme
The main goals of anti-TB therapy are:
- To cure the TB patient (by removing much of the bacilli rapidly).
- To Prevent death from, or late effects of, active-TB.
- To provide facilities for activities in training, teaching and research.
- To serve as an open institution for the prevention, control and treatment of TB and allied diseases in the region.
- To prevent the development drug resistance (by using a combination of drugs).
- To reduce the transmission of tuberculosis to others.
- To promote the national programme for the management of tuberculosis in the country and formulate strategies those are socially appropriate and economically viable to sustain and improve the programme.
- To have the country’s tuberculosis surveillance system developed.
- To ensure correct diagnosis of TB and management of treatment and further speed up the reduction of transmission of TB.
- To extend systems for adherence to tuberculosis care and touch tracing of points treated in the private sector.
Outcomes of National Tuberculosis Control Programme
In urban areas, sputum smear collection was substantially greater. In urban areas, while in tribal areas, new TB case identification was 35%; according to RNTCP (Revised National Tuberculosis Programme) requirements, it was 42%. In tribal (5.87 percentage) than urban (3 28 percentage) areas, Sputum’s positivity was slightly greater. In urban areas, the healing rate was greater than in tribal areas. In tribal areas, statistically significant high default treatment was observed.
Sputum collection and sputum positivity rates were low in urban and tribal areas, but TB screening was significantly low, particularly in tribal areas. In tribal areas, sputum positivity was substantially greater.
The need for enhancement of RNTCP activities in tribal areas is warranted by a significantly low cure rate and high default rate in tribal areas.
Make sure you also check our other amazing Article on : Drug Addiction